Table of Contents
- Why choline matters right now
- Top conditions linked to low choline
- How choline affects three big systems: liver, muscles, and brain
- Methylation, homocysteine, and why choline is often overlooked
- Acetylcholine: the forgotten neurotransmitter
- Lifestyle, convenience, and why modern living increases choline need
- Food sources of choline — what to eat
- Testing: why I insist on testing before (and while) supplementing
- Supplement forms explained and my recommendations
- Practical supplementation plan I use with clients
- Interactions and special situations
- Food, cooking, and practical tips
- Common clinical presentations that should trigger choline testing
- Answering the practical questions I get most often
- Supplements I commonly recommend and exact doses I use clinically
- Special groups: children, pregnant women, vegetarians
- When to involve a clinician
- Practical daily checklist I give clients
- Frequently asked questions
- Final thoughts and next steps
Why choline matters right now
Choline was formally declared an essential nutrient relatively recently, in 1998. Although our bodies can produce small amounts, most people cannot synthesize enough to meet physiological demands, especially under chronic stress, hormonal changes, or when liver function is compromised. Today, choline deficiency is common in modern populations for three main reasons
- Dietary patterns that favor processed foods and low-choline plant-only diets
- Increased environmental and lifestyle stressors that drain choline stores
- Limited consumer awareness and inconsistent testing for choline status
The consequence is that many people present with vague symptoms like fatigue and brain fog that are often attributed elsewhere. In reality, choline deficiency may be the missing piece.
Top conditions linked to low choline

From clinical practice and published studies, choline deficiency has been linked to:
- Non-alcoholic fatty liver disease and progressive liver injury
- Muscle breakdown, poor exercise recovery, and raised creatine kinase
- Impaired cognition and memory issues due to low acetylcholine
- Increased risk of neural tube defects and craniofacial abnormalities in pregnancy
- Higher homocysteine and associated cardiovascular risk
- Worsening insulin resistance through disrupted receptor second messenger signaling
To give you perspective from the literature, a randomized controlled deficiency study showed that when deprived of dietary choline, 77 percent of men and 80 percent of postmenopausal women developed fatty liver or muscle damage. Premenopausal women were somewhat protected but still 44 percent developed signs of organ dysfunction when dietary choline was insufficient. Those numbers explain why I routinely test for choline when I see unexplained liver enzyme elevations, persistent muscle soreness, or cognitive complaints.
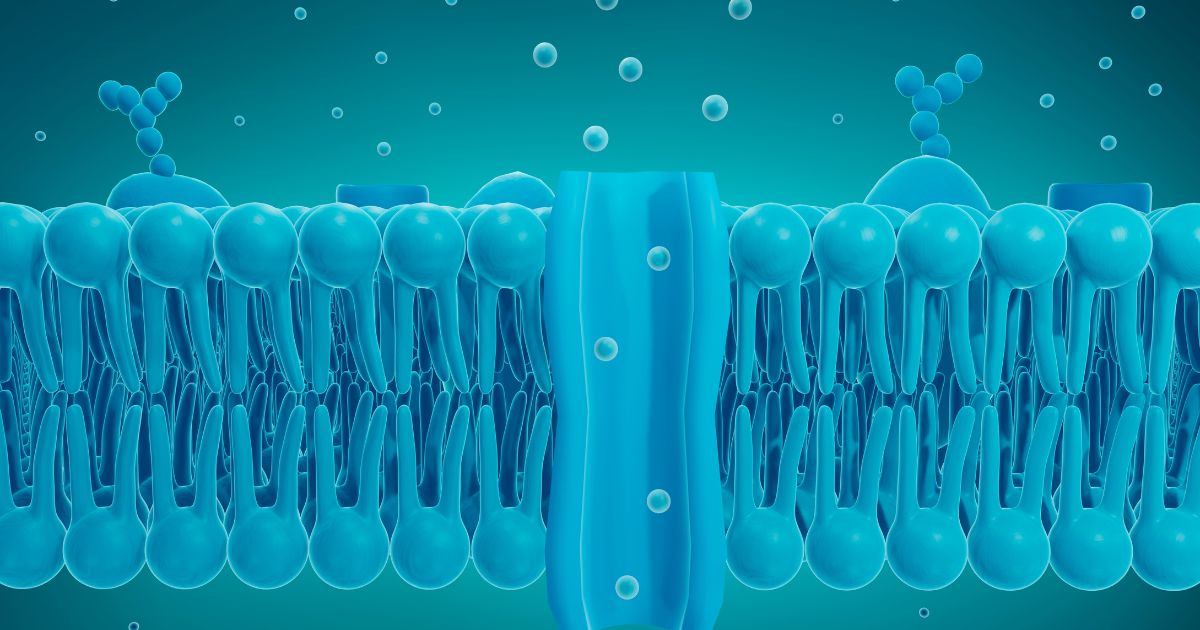
How choline affects three big systems: liver, muscles, and brain
I like to simplify choline’s actions into three major functional areas:
- Lipotropic support for the liver: choline is essential for packaging and exporting fat from the liver. Without it, fat accumulates leading to steatosis, then fibrosis and ultimately cirrhosis if uncorrected.
- Precursor for acetylcholine: choline is converted to acetylcholine, the neurotransmitter responsible for muscle contraction, parasympathetic tone, memory encoding, and neural communication.
- Methylation pathway donor: choline is converted into betaine and acts as a methyl donor to remethylate homocysteine into methionine which is a key step in DNA/RNA synthesis and repair and in maintaining cardiovascular and neurological health.
If any of these three areas are compromised, you will see clinical signs. The good news is many of these are reversible when recognized and treated appropriately.
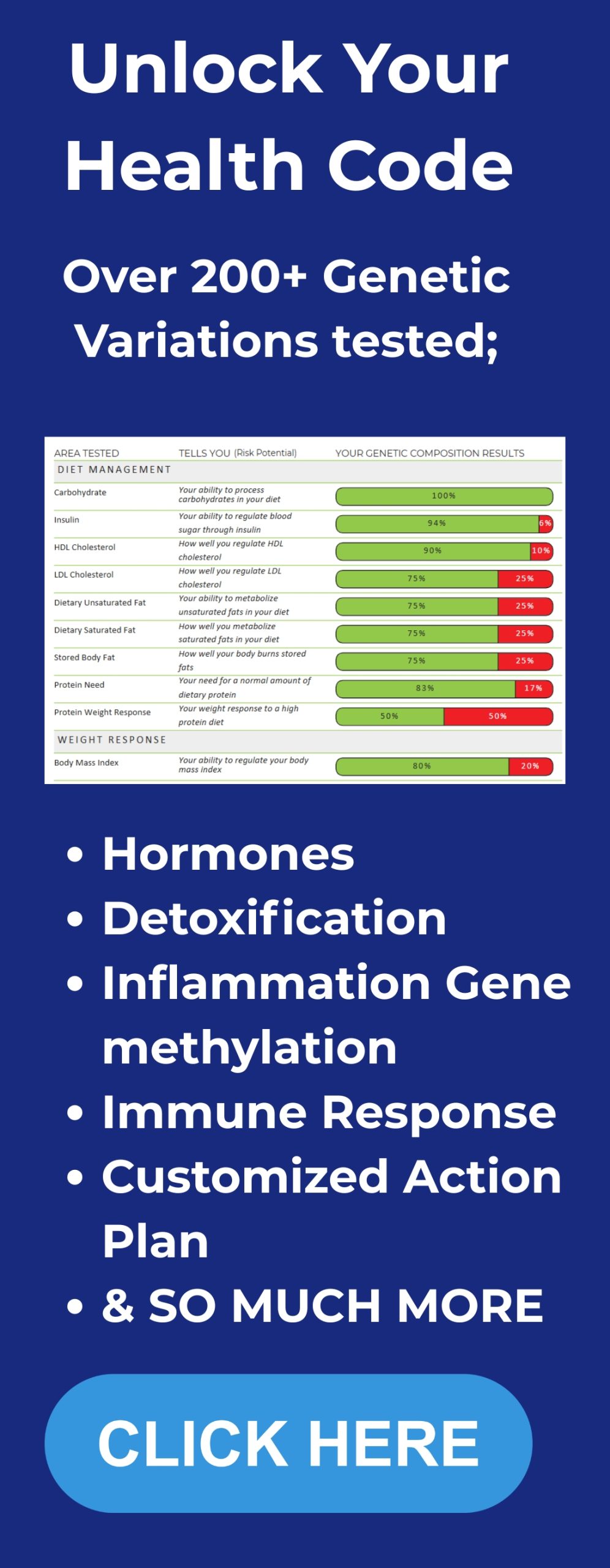
Methylation, homocysteine, and why choline is often overlooked
When people talk about methylation they usually mention folate, vitamin B12, B6, and related genes like MTHFR and MTR. To see how your unique genetic blueprint influences methylation and choline needs, consider getting personalized DNA insights. Those things are important. But choline is a major, often overlooked methylation source. Choline is converted to betaine (trimethylglycine), which donates methyl groups to convert homocysteine into methionine. Elevated homocysteine is an independent risk factor for stroke, heart disease, type 2 diabetes, certain cancers, and osteoporosis. My practical target for homocysteine is less than 9 micromoles per liter with an ideal range roughly 5 to 9.
Which nutrients lower homocysteine? Folate and B12 via remethylation, B6 via the transsulfuration pathway to glutathione, B2 and riboflavin for several enzymatic reactions, choline/betaine, and supplementally SAMe or methionine in targeted circumstances. The right combination depends on what the testing shows, which is why I insist on testing rather than blind supplementation.
Acetylcholine: the forgotten neurotransmitter
Acetylcholine derived from choline is foundational to nervous system work. Two clinical areas I watch closely are cognition and autonomic balance.
- Cognition and memory: acetylcholine is the main neurotransmitter for memory formation and for neurons to communicate efficiently. Choline deficiency can present as fatigue, brain fog, mood instability, and long-term risks for cognitive decline.
- Muscle contraction and neuromuscular health: acetylcholine enables nerves to tell muscles to contract. Chronic low acetylcholine impairs neuromuscular signaling and can lead to muscle atrophy, elevated CK, and persistent soreness with poor recovery.
- Parasympathetic tone and the vagus nerve: acetylcholine is the main chemical used by the parasympathetic system to regulate digestion, sleep, gallbladder contraction, salivation, heart rate, and calming down adrenaline production. When choline is low you are literally sabotaging your vagus nerve signaling and locking yourself into a chronic sympathetic dominant state.
Lifestyle, convenience, and why modern living increases choline need
Modern life has created chronic low-level stressors that force our bodies to use up more choline. Here are the main drivers I see:
- Processed and convenience foods that lack nutrient density
- Viral infections and inflammation that increase repair demands
- Environmental toxicants and gut dysbiosis that worsen hepatic processing needs
- High EMF and chronic technology exposure that bias the nervous system toward sympathetic tone
- Hormonal transitions such as menopause, which reduce estrogen-mediated choline protection and elevate choline requirements
Because choline supports cell membranes, hormone receptor sensitivity, and second messenger systems, poor diet and chronic stress magnify the problem. You can make progress by addressing both the drains and the replenishment.
Food sources of choline & what to eat
I always start with food-first. Here are the highest choline-containing foods I recommend. Rotate them rather than relying on a single source like eggs
- Egg yolks — one of the richest and most bioavailable sources (why I often recommend eating multiple eggs per day)
- Liver — beef or chicken liver is exceptionally rich in choline
- Fish roe or caviar and fatty fish like salmon
- Beef, pork, chicken, and turkey
- Soy lecithin or sunflower lecithin derived phosphatidylcholine — use organic sunflower-derived if you choose
- Brassica vegetables — cauliflower, broccoli, Brussels sprouts (plant sources contain choline but in smaller amounts)
- Shiitake mushrooms and certain nuts and seeds

Important note for vegetarians and vegans: a strictly plant-based diet increases risk of choline deficiency because the richest sources are animal based. If you follow a plant-only approach, be intentional about the highest plant sources and consider testing and supplementation. Pregnant and breastfeeding women especially need to be vigilant since choline is necessary for fetal brain development and to prevent neural tube defects.
Testing: why I insist on testing before (and while) supplementing
Testing removes guesswork. The tests I use most often:
- Serum homocysteine — quick and informative for methylation stress
- Intracellular choline when available — this gives the best indication of cellular choline stores
- Liver enzymes ALT and AST and a comprehensive metabolic panel — to assess hepatic function
- TMAO level if you’re concerned about gut dysbiosis and cardiovascular risk
- Creatine kinase with isoenzymes — to determine if elevated CK is muscle, heart, or brain derived
- Comprehensive micronutrient panel including B12, folate, B6, B2, magnesium
Why intracellular choline? Blood levels alone are misleading because they do not reflect cellular stores. Intracellular measures, when available through specialized labs, guide therapeutic dosing. I use testing to tailor the plan and then retest after 8 to 12 weeks of intervention.
Supplement forms explained and my recommendations
Not all choline supplements are created equal. There are three common supplement forms you will encounter:
- Phosphatidylcholine (lecithin based) — a fat soluble form usually derived from soy lecithin or sunflower lecithin. Pros: a natural membrane phospholipid; cons: if derived from non-organic soy it may carry pesticides or GMOs. Also, because it reaches the colon it can be converted by some gut bacteria into trimethylamine oxide TMAO in susceptible microbiomes.
- CDP-choline or citicoline — marketed for brain support. It can be helpful for cognitive symptoms but many products have a low percent choline by weight because of the carrier molecules. It is not the most efficient way to raise systemic choline when the liver or methylation needs are primary.
- Choline bitartrate — a cheap, common form often derived from corn. If you are following a strict grain-free or no-grain-no-pain protocol, avoid it. Also many find it less bioavailable for therapeutic dosing.
- Choline citrate — my preferred form for systemic repletion. It provides a high percent choline, is alkalinizing due to the citrate carrier, improves magnesium uptake at the cellular level, and is absorbed in the stomach and upper small intestine. Because it is absorbed before reaching the colon, it minimizes conversion to TMAO.
My go-to recommendation for supplementation:
- Choline citrate — start with 250 to 350 mg elemental choline daily as a maintenance dose for someone with mild symptoms or to support baseline needs.
- If testing shows deficiency or if you have fatty liver, elevated homocysteine, persistent elevated CK, or marked cognitive symptoms, target 500 to 700 mg elemental choline daily for therapeutic repletion until re-testing. I commonly use 500 mg twice daily for a short course in severe deficiency cases, but only under supervision and after baseline labs.
- For daily long term maintenance many people do well on 250 to 500 mg/day depending on diet and stressors.
I want to be clear, the numbers above refer to elemental choline not total product weight. Check supplement labels for elemental choline amounts. If you buy a product marketed as choline citrate, verify the mg of choline per serving.
Why I prefer choline citrate
Choline citrate has several practical advantages:
- It is generally grain free and not corn derived like choline bitartrate.
- Citrate supports intracellular pH balance and helps improve magnesium uptake, which is critical because many people are intracellularly magnesium deficient.
- Choline citrate is absorbed in upper GI rather than delivered in large amounts to the colon where certain bacteria can convert choline into TMAO.
- It can be formulated in a liquid so you can reach therapeutic doses without dozens of pills.
When choosing any supplement, prioritize third-party tested brands, organic or non-GMO sources when possible, and transparent labeling that lists elemental choline.
Practical supplementation plan I use with clients
Below is a structured protocol I use at BetterLife when a client has confirmed choline deficiency or a clinical picture consistent with deficiency. This is an example plan; individual needs vary and I always monitor labs.
Initial assessment
- Baseline labs: CMP including ALT AST, fasting lipid panel, homocysteine, intracellular choline if available, CK isoenzymes, ferritin, CBC, magnesium RBC or intracellular magnesium, thyroid panel
- Dietary history and GI symptom review
- Medication review (for example methotrexate use or other drugs that interfere with methylation)
Short term corrective phase (8 to 12 weeks)
- Choline citrate: 500 mg elemental choline twice daily with meals for 8 weeks if severe deficiency or liver involvement. If moderate deficiency use 500 mg once daily for 8 to 12 weeks.
- Magnesium citrate or glycinate: 200 to 400 mg elemental magnesium at night. Adjust depending on baseline magnesium testing and tolerance. Combining choline citrate helps magnesium get into cells more effectively. See our BetterLife VIP protocol essentials including CanPrev’s Magnesium for practitioner-selected options.
- Methylated B complex: a daily B complex that includes methylfolate 400 to 800 mcg, methylcobalamin 1000 mcg, B6 pyridoxal-5-phosphate 25 to 50 mg, riboflavin 5 to 10 mg. These support methylation and homocysteine lowering.
- Consider betaine anhydrous 500 mg twice daily in specific cases where homocysteine remains high despite other measures. Use only under practitioner guidance.
- SAMe 200 to 400 mg daily can be considered in some cases to support methylation and mood; use cautiously and not combined with certain antidepressants without guidance.
- Address gut health aggressively if TMAO elevated; probiotics, antimicrobial strategies, or targeted microbiome therapy may be required.
Maintenance phase
- Choline citrate 250 to 500 mg daily depending on diet and symptoms
- Daily magnesium 200 to 300 mg if deficient or symptomatic
- Multivitamin with methylated B12 and folate
- Yearly or periodic re-testing of homocysteine, liver enzymes, and intracellular choline as clinically indicated
Always re-evaluate symptoms and labs at 8 to 12 weeks. If liver enzymes normalize and homocysteine is in range, step down to maintenance dosing.
Interactions and special situations
Methotrexate and autoimmune arthritis
Methotrexate inhibits methylation and is known to cause liver damage in some patients. Clinically, supplementing folate is common, but choline is rarely added despite evidence that choline can ameliorate methotrexate-induced liver damage. If you take methotrexate discuss choline supplementation with your prescribing physician and involve a provider who understands nutrient-drug interactions. Typical approach is to use choline citrate in therapeutic doses while monitoring liver enzymes.
Pregnancy and fetal development
Choline is critical in pregnancy for neural tube development, brain formation, and preventing cleft palate and other craniofacial defects. Pregnancy increases choline needs and many practitioners recommend ensuring you meet or exceed the recommended intake during pregnancy, often through combined diet and supplementation. Work with your OB or integrative practitioner and test homocysteine and related markers.
Cardiovascular concerns and TMAO
TMAO formation happens when certain gut bacteria metabolize phosphatidylcholine and carnitine into trimethylamine, which gets oxidized in the liver to TMAO. Elevated TMAO has been associated with cardiovascular risk in some studies. However, the main driver of elevated TMAO is gut dysbiosis rather than meat consumption alone. If your TMAO is high, address microbiome balance first and consider choline citrate rather than phosphatidylcholine to minimize colonic conversion.
Iodine and thyroid testing
Iodine is protective in radiation exposure and is an important nutrient for thyroid function. A note of caution: high doses of iodine can artificially elevate TSH when measured, and in some people taking iodine mobilizes stored halides like bromine and fluoride which can temporarily cause symptoms. If you take higher doses of iodine and your TSH becomes unexpectedly high, stop iodine for two weeks and recheck before making thyroid medication changes. Always coordinate with your physician.
Food, cooking, and practical tips
Yes you can eat eggs every day if you are not allergic. Cook them however you like, hard boiled, scrambled, fried in a healthy oil. Raw eggs carry a small risk of salmonella and contain avidin, a protein that in very high raw-egg diets can impair biotin absorption. So I recommend cooking eggs and getting variety in your diet rather than relying on one single source.
If you are vegetarian or vegan and have hypothyroidism and have been told to avoid brassica vegetables, realize those same foods are some of the few reasonable plant sources of choline. If you avoid brassicas and animal foods you may fall short quickly in choline, especially during perimenopause or menopause. In those situations, be proactive about testing and consider supplementation.
Common clinical presentations that should trigger choline testing
- Mild to moderate elevation in ALT and AST without alcohol use
- Persistent muscle aches, elevated CK, poor recovery from exercise
- Fatigue, brain fog, short term memory loss, and mood instability
- Elevated homocysteine despite B vitamin supplementation
- Pulled into vegan or low-animal diets and experiencing new cognitive or liver symptoms
- People on methotrexate or other methylation inhibitors
Answering the practical questions I get most often
How much choline do I personally take?
On maintenance I take 140 mg of supplemental choline daily as a baseline but this is supplemental on top of a diet that includes egg yolks and other choline-rich foods. If I’m treating a client with clear deficiency, I raise to therapeutic doses as outlined above and retest.
Is lecithin an antidote to cholesterol?
Lecithin contains phosphatidylcholine and plays a role in healthy lipid handling by the liver. It helps the liver package lipids and can improve the way cholesterol is processed. I agree with the general principle that a lipotropic like lecithin can be supportive of healthy cholesterol metabolism when used appropriately.
Which B vitamins should I take with choline?
Take a methylated B complex that includes methylfolate, methylcobalamin, active B6, and riboflavin. These work synergistically with choline on methylation and homocysteine removal. Standard starting dosing I commonly use:
- Methylfolate 400 to 800 mcg daily
- Methylcobalamin 1000 mcg sublingual daily for those with absorption issues or low serum B12
- Pyridoxal-5-phosphate 25 to 50 mg daily
- Riboflavin 5 to 10 mg daily
Will choline supplementation worsen TMAO?
Not if you choose the right form. Phosphatidylcholine and lecithin can be metabolized by gut bacteria into TMAO in dysbiotic guts. Choline citrate is absorbed before the colon and therefore greatly reduces the risk of TMAO production from supplemental choline.
How to handle elevated homocysteine
Homocysteine typically responds to a combination of nutritional interventions tailored to testing. My order of operations:
- Confirm actual status with a lab test
- Ensure you have adequate B12 and folate in the right forms
- Add choline/betaine support if indicated
- Correct magnesium and B6 as needed
- Address kidney function because renal impairment can keep homocysteine high even with supplements
Supplements I commonly recommend and exact doses I use clinically

Below is a consolidated list you can use to discuss with your clinician. This is not medical advice but a summary of what I use in practice.
- Choline citrate — maintenance 250 to 350 mg elemental choline daily; therapeutic 500 to 700 mg daily divided BID if deficiency or liver disease is present; use liquid formulation if high dosing needed.
- Magnesium citrate or glycinate — 200 to 400 mg elemental magnesium nightly; titrate based on RBC magnesium testing and bowel tolerance.
- Methylated B complex — methylfolate 400 to 800 mcg, methylcobalamin 1000 mcg sublingual, P5P 25 to 50 mg, riboflavin 5 to 10 mg.
- SAMe — 200 to 400 mg daily selectively for methylation or mood support when indicated.
- Betaine anhydrous — 500 mg twice daily in selected homocysteine cases under supervision.
- Creatine monohydrate — 5 g daily for muscle building and recovery; optional loading 20 to 25 g daily for 5 to 7 days followed by 5 g/day.
- Iodine — physiological dosing via diet or supplement; I keep an iodine product available for higher risk travel but caution monitoring TSH when dosing high. Typical supplemental iodine protocols vary widely; work with a clinician.
- Omega-3s — target daily intake of EPA and DHA combined depending on clinical need, or use grass-fed beef and fish; if allergic to fish explore molecular distillate or algae-derived DHA/EPA.
Special groups: children, pregnant women, vegetarians
Children need adequate animal source nutrients for growth. I do not advocate strict vegan diets for growing children without careful planning, testing, and supplementation. Pregnant and breastfeeding women need increased choline and some practitioners recommend meeting or exceeding the recommended intake through diet and supplementation because fetal brain development depends on adequate choline.
Vegetarians and vegans should monitor choline and arrange targeted testing because plant-based sources often fall short, especially during hormonal transitions. If you are a female entering perimenopause or menopause, choline needs rise and dietary gaps show up clinically.
When to involve a clinician
If you have any of the following, seek medical advice before starting high-dose choline or other targeted therapies:
- Known liver disease or cirrhosis
- Being on medications that affect methylation such as methotrexate
- Significant kidney disease
- Severe cardiovascular disease or recent cardiac event
- Pregnancy — coordinate with your OB
Practical daily checklist I give clients
- Eat one to two servings of high choline foods daily: egg yolks, small serving of liver weekly, fatty fish or quality meats.
- Take choline citrate supplement as per testing and symptoms.
- Include a methylated B complex daily.
- Ensure 200 to 400 mg magnesium nightly.
- Address gut health if you have chronic digestive symptoms before assuming all elevated TMAO is dietary.
- Get labs: homocysteine, ALT AST, CK isoenzymes, intracellular magnesium, and intracellular choline when available.
- Prioritize sleep, whole foods, sunshine, clean water and air, and stress reduction to reduce choline drain.
Frequently asked questions
Can I take B and C vitamins together?
Yes. B vitamins and vitamin C can be taken together; they do not interfere with one another and are commonly included together in multi formulas.
Will choline cause muscle cramps?
Choline deficiency can cause muscle cramps and electrolyte imbalances via kidney handling of electrolytes. Correcting choline and magnesium together often resolves cramps.
Are eggs safe to eat raw for choline?
Raw eggs carry a small risk of Salmonella and raw egg avidin can impair biotin in high quantities. Cook your eggs to reduce risk and combine with other choline sources for best practice.
Is whey protein recommended to gain muscle?
Most commercial whey protein is heat processed and often made from A1 dairy which some people avoid. Creatine monohydrate at 3 to 5 g daily is an excellent and safe way to build strength. For protein, choose high quality sources; if you need a product I recommend, check BetterLifeProtocols.com for our vetted options.
How do I reduce elevated TMAO?
Address gut dysbiosis first. Work with a clinician to assess microbiome composition, treat overgrowth or imbalances, and then prefer choline citrate over phosphatidylcholine to minimize colonic conversion to TMAO.
What labs should my doctor order to evaluate choline related issues?
Request homocysteine, ALT, AST, CK with isoenzymes, a comprehensive micronutrient panel, RBC magnesium or intracellular magnesium, and if available intracellular choline. For gut-related TMAO concerns ask for a TMAO test.
Final thoughts and next steps
Choline sits at the crossroads of liver health, brain function, muscle integrity and methylation. Because it is both synthetically produced to some degree and diet-dependent, many people assume they are fine. In my practice I see the opposite. Testing changes everything. Before you assume any symptom is unrelated to nutrition, check choline related markers and homocysteine. If you are low that creates a clear path forward: food first, targeted supplementation with choline citrate when indicated, correction of magnesium and B vitamins, and reassessment with labs.
If you’re ready to take action, the best approach is to integrate testing, diet, and supplementation into a clear plan. That’s exactly what we do with our Integrate program where we focus on guiding you step by step so you don’t have to guess.