Today we’re diving into one of the most fascinating compounds being studied for mental health and brain function: psilocybin. While most people know it as the active ingredient in so-called “magic mushrooms,” researchers are uncovering an impressive range of therapeutic possibilities that extend far beyond its reputation. From reshaping neural circuits and enhancing brain plasticity to showing promise for conditions like depression, anxiety, and addiction, psilocybin is rapidly becoming one of the most exciting frontiers in neuroscience and clinical therapy.
In this post, we’ll explore the science-backed reasons why psilocybin is attracting so much attention and what it is chemically, how it works in the brain, why clinicians are optimistic about its potential, and what a typical session looks like in a supervised or clinical setting. We’ll also look at strategies for managing acute anxiety during a session and highlight evidence-based supplements and practices that can support both preparation and integration. Let’s take a closer look at the research and see why psilocybin is generating so much excitement in the world of mental health.
Table of Contents
- What Psilocybin Is — the chemistry in plain language
- Why 5-HT2A matters — receptor location and functional consequence
- From molecule to experience — a short chain of events
- What a psilocybin journey typically looks like — timing and phases
- Set and setting — how context changes outcomes
- Subjective experiences that predict therapeutic benefit
- How psilocybin changes brain networks — integration, not chaos
- Cellular neuroplasticity — dendritic growth and the addition of spines
- What psilocybin does not primarily do: neurogenesis
- Translating mushroom grams to milligrams — dosing explained
- Clinical evidence — what conditions have proven effects?
- Who should not take psilocybin
- Practical pre-session and post-session guidance — my recommended protocol
- Supplements, vitamins, and exact dosages I recommend for safety and to support neuroplasticity
- Why support with sleep, exercise, and targeted supplements matters
- FAQ — Practical questions answered
- Final thoughts and guiding principles
What Psilocybin Is — the chemistry in plain language

Psilocybin belongs to a family of molecules called tryptamines. That label refers to the chemical scaffold the molecule is built from. Tryptamines include compounds such as DMT and 5-MeO-DMT and are chemically similar to serotonin, the brain’s major neuromodulator. When you take psilocybin orally it is converted in the gut into psilocin the active form that crosses into the brain and binds to serotonin receptors.
Because psilocin so closely resembles serotonin, the brain’s serotonin receptors interpret psilocin similarly to serotonin. That similarity explains why psilocin has such a powerful and broad effect on perception, mood, and cognition. But psilocin is selective: it strongly activates a specific subtype of serotonin receptor known as the serotonin 2A receptor or 5-HT2A. That receptor’s location and function explain most of the unique effects people experience on psilocybin.
Why 5-HT2A matters — receptor location and functional consequence
5-HT2A receptors are abundant in parts of the cortex, especially the neocortex. They’re heavily expressed in frontal regions involved in context, planning, and regulation of behavior, and they are highly expressed in primary sensory cortices, most notably the visual cortex. Activation of 5-HT2A receptors on certain cells leads to dramatic changes in how brain areas talk to one another.
That localization explains several common effects of psilocybin. Visual hallucinations relate in large part to activation of 5-HT2A receptors in visual cortex. Changes to self-related processing and cognition relate to activation in frontal cortex and networks that support self-representation and spontaneous thought.
From molecule to experience — a short chain of events
- Ingestion (or oral dosing of synthetic psilocybin).
- Conversion in the gut to psilocin, the active ligand that crosses the blood brain barrier.
- Psilocin binds with high potency to 5-HT2A receptors, especially on apical dendrites of cortical pyramidal neurons.
- Activation of 5-HT2A receptors changes neuronal excitability and intracellular signaling pathways that promote growth, spine formation, and altered network communication.
- Subjective effects: altered sensory perception, synesthesia, changes in thought patterns, emotional shifts, and at times intense anxiety and ego dissolution during the peak.
What a psilocybin journey typically looks like — timing and phases

A typical supervised psilocybin session lasts four to six hours from onset to resolution. Key phases:
- Onset: 20 to 60 minutes after dosing — subtle perceptual changes, mood shifts.
- Ascent to peak: often between 60 and 120 minutes — perceptual blending, increased emotional intensity.
- Peak: pronounced changes in perception, frequently associated with the greatest emotional intensity and sometimes acute anxiety or fear. This is when feelings like ego dissolution and oceanic boundlessness most commonly occur.
- Descent and integration: hours two through six — emotions and perceptions phase down and the person returns to baseline awareness; the brain is primed for plasticity in the hours to days afterward.
Set and setting — how context changes outcomes
Set refers to mindset which is a person’s intentions, expectations, and mental state going into the session. Setting refers to the physical and social environment like the room, the people present, whether the participant is lying down or walking in nature, whether music is played, etc. Clinical evidence shows both matter greatly.
Key features that clinical trials consistently use and that are associated with better outcomes:
- Supervised environment with at least one trained, sober guide present.
- Closed, safe room without windows that could create danger. The emphasis is safety first.
- Opportunity and bias toward lying down with an eye mask for the majority of the session so inward experiences are emphasized over outside stimuli; most effective clinical protocols favor eyes closed for most of the journey.
- Structured music playlists that rise and fall with the session rhythm: calm, instrumental music early; more rhythmic, percussive and intense music during the peak; and softer, melodic or nature-oriented music during descent and return.
- Pre-session psychological preparation and post-session integration therapy or counseling.
Subjective experiences that predict therapeutic benefit
Clinical researchers have quantified subjective aspects of the session and correlated them with downstream therapeutic results. Two important constructs are:
- Oceanic boundlessness — a mystical-like sense of expansive connection, unity, and profound insight. Higher intensity of this experience correlates with better long-term outcomes for depression.
- Ego dissolution and letting go — many participants describe a forced or voluntary “letting go” of habitual self-narratives. Successfully moving through the peak and returning from ego dissolution is associated with therapeutic gains.
However, there is nuance. An acute peak that is overwhelmingly anxious correlates with poorer outcome. A moderate-to-high intensity peak with guidance and tools to manage anxiety, and with an eventual sense of insight or connectedness, appears to be the most therapeutically potent combination.
How psilocybin changes brain networks — integration, not chaos

At a systems level, psilocin binding to 5-HT2A receptors changes the brain’s communication patterns. Key features that research has observed with neuroimaging and electrophysiology:
- Reduced modularity and increased global integration. Brain areas that normally operate more independently start to communicate more broadly with one another. That’s why auditory, visual, and interoceptive signals may blend (synesthesia).
- Reduced hierarchical gating from the thalamus, meaning bottom-up sensory signals have broader access to higher-order centers and vice versa. That creates conditions for new associations and novel insights.
- Disruption or modulation of the default mode network, the system associated with self-referential thought, which correlates with ego dissolution experiences.
- Some of the expanded connectivity persists beyond the acute effects of the drug, which likely underlies the long-term therapeutic effects.
Cellular neuroplasticity — dendritic growth and the addition of spines
Important mechanistic data comes from animal models and a growing body of human imaging studies. The predominant cellular processes associated with psilocybin-induced plasticity are structural changes to existing neurons rather than massive generation of new neurons. The key events include:
- Growth of dendritic branches and apical tufts on pyramidal neurons in cortex.
- The rapid formation of dendritic spines — small mushroom-shaped protrusions on dendrites that serve as the primary sites of excitatory synaptic input.
- These spine additions can persist long after the drug has cleared in animal models, suggesting a structural basis for enduring change.
One high-profile animal study demonstrated rapid and persistent spine growth in the frontal cortex following a single psilocybin exposure. That result aligns conceptually with postmortem human data showing reduced spine density in certain cortical areas in depressed individuals. Thus, spine growth may be one of the biological mechanisms underlying mood improvement after psilocybin-assisted therapy.
What psilocybin does not primarily do: neurogenesis
There’s often confusion about whether psychedelics cause new neurons to be born in adult cortex. The dominant evidence suggests adult neurogenesis is a very limited contributor to human cortical plasticity. The larger, better-supported mechanisms are changes in dendritic structure and synaptic connectivity. So when people talk about psilocybin “rewiring” the brain, they mostly mean new synaptic connections and altered network communication rather than wholesale addition of new neurons.
Translating mushroom grams to milligrams — dosing explained

If you’re converting mushrooms to psilocybin milligrams, here is a useful rule-of-thumb clinicians and researchers tend to use:
- Most so-called magic mushrooms contain roughly 0.5 to 2 percent psilocybin by dry weight. A common central estimate is ~1 percent.
- 1 gram of dried mushrooms ≈ 10 mg of psilocybin (if 1 percent)
- Clinical therapeutic doses most commonly studied: 25 to 30 mg of psilocybin (typically given as a synthetic, standardized dose) — this is frequently the dose associated with significant improvements in treatment-resistant depression.
- 10 mg is a lower clinical dose used sometimes for familiarization.
- Microdosing in research contexts is usually 1 to 3 mg per day when given repeatedly for extended intervals; that is distinct from the single-session therapeutic doses described above.
- A so-called “heroic” dose in informal psychonaut communities often refers to about 50 mg psilocybin, which corresponds roughly to 5 grams of dried mushrooms; this is substantially higher than most clinical protocols.
Important caveats about mushrooms: psilocybin concentration varies widely across strains and batches and depends on growing, storage, and drying conditions. That’s another reason clinical trials use synthetic psilocybin: to control dose precisely.
Clinical evidence — what conditions have proven effects?
Over the past decade there has been a rapid increase in high-quality randomized trials and controlled studies. The strongest evidence currently exists for:
- Treatment-resistant depression — multiple randomized trials have shown substantial improvements in depression measures after one or two supervised psilocybin sessions at therapeutic doses, with many participants demonstrating sustained improvement out to weeks and months after dosing.
- Cancer-related anxiety and depression — controlled trials report meaningful reductions in existential anxiety and depressive symptoms.
- Addiction support — early trials for tobacco cessation and alcohol use disorder show promise but are less conclusive than the depression data.
Who should not take psilocybin
- People with a personal or close family history of schizophrenia or a primary psychotic disorder.
- People with active bipolar I or a history of mania.
- People under age 25 in most clinical protocols.
- Pregnant or breastfeeding women.
- People who cannot ensure a supervised, safe environment with trained guides.
- People for whom stopping current psychiatric meds would be unsafe.
Practical pre-session and post-session guidance — my recommended protocol
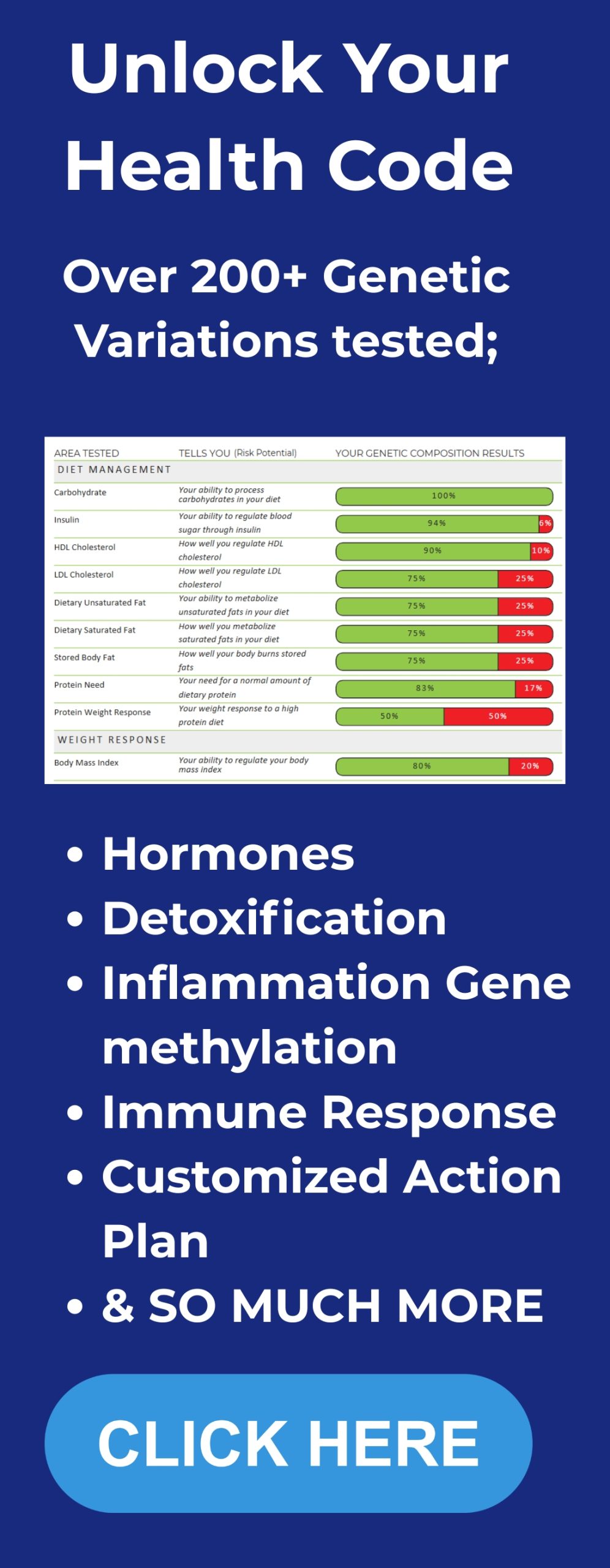
Below is a practical checklist intended for educational purposes only. This is not medical advice. Always consult licensed professionals and the team running a clinical trial or licensed therapeutic program. Everyone’s biology is different, and tailoring your approach can make a big difference. Get personalized DNA-based health insights here to better align supplements and recovery strategies with your genetics.
Two to four weeks before the session
- Medical and psychiatric screening with a licensed clinician: confirm no contraindicated psychiatric history, family history of psychosis, and check cardiovascular status.
- If on antidepressants: consult prescribing psychiatrist about supervised taper options — never abruptly stop medication without clinical guidance.
- Begin gentle sleep optimization: consistent schedule and temperature regulation at night; consider tools that help you keep your core temperature lower and support restorative sleep.
- Start journaling to build intention and identify key themes you may want to explore during the session.
48 to 24 hours before the session
- Avoid alcohol and recreational drugs.
- Avoid cannabis for at least 48 hours prior; cannabis alters anxiety and perception unpredictably.
- Eat light the day before; clinical protocols typically ask for no heavy meals within 4 hours before dosing.
- Hydrate and consider electrolyte balance the day before (see supplement section below).
Day of session
- Ensure you have a sober, trained guide or session team present.
- Bring a blanket, comfortable clothing, and an eye mask. Lie down if recommended; most trials have participants lie down with eyes closed for most of the session.
- Practice the physiological sigh and other grounding strategies beforehand so you know them under stress.
- Do not drive for 24 hours after the session and ensure a trusted person escorts you home if needed.
After the session — integration
- Plan multiple integration sessions with a trained therapist or counselor in the following days and weeks. Many clinical protocols include 8–12 hours of structured integration over several weeks. Read more about structured Integrate protocol here.
- Prioritize sleep, gentle movement (walking, yoga), and social connection.
- Use journaling, art, or music to capture insights; repeat exposure to music that was meaningful during the session can reinforce positive emotional rewiring.
- Maintain physical health and nutrition to support plasticity: regular exercise, adequate protein, sleep, and controlled stress exposure.
Supplements, vitamins, and exact dosages I recommend for safety and to support neuroplasticity
Below I list supplements and dosages I typically recommend for adults pursuing a supervised, clinical psilocybin experience. These are suggestions for general supportive care and are not a guarantee of safety or efficacy. Always consult your prescribing physician, psychiatrist, or the clinical team running the session before starting or stopping supplements, particularly anything that impacts serotonin, blood pressure, or anticoagulation.
Baseline daily foundational supplements (long-term)
- Vitamin D3: 2,000 to 5,000 IU daily with Vitamin K2 (MK-7) 100 mcg daily. Supports immune regulation, mood, and general health. Have blood levels checked (25(OH)D target range 30 to 60 ng/mL) and adjust dosage accordingly. Learn more about why Vitamin D is essential here.
- Omega-3 fish oil (EPA+DHA): 1,000 to 2,000 mg combined EPA+DHA daily. High-quality triglyceride form is preferred. Omega-3s support neuronal membrane integrity and may augment plasticity. Explore high-quality foundational supplements including Omega-3s here.
- Magnesium (glycinate or threonate): 200 to 400 mg nightly. Magnesium supports sleep quality, reduces hyperexcitability, and is commonly used to promote calmness. Take at night to reduce GI side effects and to support sleep. Not all magnesium is created equal — discover why some forms are better absorbed here.
- Probiotic: a multi-strain probiotic once daily — or a nutritional product that includes probiotics and prebiotics (one serving daily). Gut health modulates inflammation and can influence mood via the gut-brain axis.
- B-complex: a quality B-complex once daily with recommended label dosing if you have elevated stress or are adjusting sleep. Avoid high-dose B6 for prolonged periods unless advised by a clinician.
Peri-session recommendations (days before, day of, and after)
- Electrolytes: Maintain good hydration and electrolyte balance. A clinical-grade electrolyte mix with approximately 1,000 mg sodium, 200 mg potassium, and 60 mg magnesium per serving is a practical option to take the morning of the session and in the days after if you feel dehydrated. One serving in the morning of the session is typical unless the clinical team directs otherwise.
- Avoid serotonergic supplements: Do not take 5-HTP, St John’s Wort, tryptophan, or other supplements that directly increase serotonin without direct clinical advice. These may alter serotonin receptor sensitivity and interact with serotonergic medications.
- Avoid MAOIs: Monoamine oxidase inhibitors interact dangerously with many compounds and foods. Do not take any MAOI herbs or drugs without supervised medical oversight.
Optional adjuncts to consider with medical guidance
- Lion’s Mane mushroom extract: 500 to 1,000 mg twice daily is commonly used in research and community protocols to support neurotrophic signaling and cognition. The evidence is preliminary but promising for supporting neural health. Use only under guidance if you have allergies or on immunosuppressive medication.
- Curcumin (with piperine for absorption): 500 mg twice daily. Curcumin has anti-inflammatory and neuroprotective effects. Nice adjunct for broad brain health but avoid if you have active gallbladder disease or are on certain anticoagulants unless cleared by a clinician.
- Creatine monohydrate: 3 to 5 grams daily. Creatine supports cellular energetics, including neuronal energy metabolism, and is safe for most healthy adults. Check kidney function with your doctor if you have kidney disease.
Important safety notes about supplements:
- If you’re on blood thinners, antiplatelet therapy, or have bleeding disorders, discuss fish oil and curcumin with your doctor as they can affect bleeding risk at higher doses.
- Do not start or stop prescription medications in the peri-session window without direct medical supervision from the prescribing clinician.
Why support with sleep, exercise, and targeted supplements matters
Psilocybin initiates a window of enhanced plasticity. To make plasticity adaptive, you need to pair that window with the right behaviors: adequate sleep, emotional processing (therapy), structured behavior change, learning, creativity practice, and social supports. Supplements can help optimize sleep, inflammation, and neural metabolism so that the structural changes the drug initiates are more likely to consolidate in useful ways.
FAQ — Practical questions answered
Q: Is psilocybin the same as psilocin?
A: No. Psilocybin is a prodrug. After ingestion psilocybin is dephosphorylated to psilocin in the gut; psilocin is the molecule that crosses into the brain and binds to 5-HT2A receptors.
Q: How long do therapeutic benefits last?
A: Durable improvements are reported in many participants for weeks to months after a supervised session. Some participants report changes that persist for many months to beyond one year, but longitudinal data are ongoing. Benefits often depend on follow-up integration and life changes after the session.
Q: What dose is typically used in clinical trials?
A: Common therapeutic doses are 25 to 30 mg of synthetic psilocybin in a single session, sometimes repeated for a second session. Lower doses such as 10 mg are used for familiarization. Microdoses in trials are often 1 to 3 mg daily and are a separate paradigm with different goals.
Q: Can I microdose and expect the same outcomes as supervised therapeutic dosing?
A: No. Microdosing protocols aim for subtle daily effects on mood or cognition. Most large clinical improvements in treatment-resistant depression reported in the literature come from one or two supervised macrodoses, not from microdosing.
Q: What supplements are critical around a session?
A: The most practical supports are ensuring adequate Vitamin D status, omega-3 intake (EPA + DHA ~1–2 g/day), magnesium (200–400 mg nightly), a quality probiotic, and maintaining electrolyte balance (for example an electrolyte mix with ~1 g sodium, ~200 mg potassium, and ~60 mg magnesium if indicated). Avoid serotonergic supplements like 5-HTP unless advised by your treating psychiatrist.
Q: How do I manage a bad trip?
A: If in a supervised setting, trained guides use grounding, reassurance, breathing techniques like the physiological sigh, and environmental modifications (reduce noise, increase lighting control, provide a weighted blanket) to help. In unsupervised settings the risk is higher — that’s why clinical supervision is strongly recommended.
Q: Should young people under 25 use psilocybin?
A: Most clinical trials do not include participants under 25. The adolescent and early adult brain is still undergoing developmental plasticity. Clinical safety and efficacy in that group require careful study; current guidance is generally conservative and favors delaying psychedelic therapy until adulthood unless under specialized clinical research protocols.
Q: Can psilocybin cause long-term cognitive deficits?
A: High-quality clinical trials have not shown persistent memory impairment as a common outcome. Rather, for many participants, cognition and emotional responsiveness improve. However, isolated adverse outcomes can occur, particularly in unscreened populations or when combined with other risky behaviors.
Q: Can I combine psilocybin with my antidepressant?
A: Most trials have required participants to taper off serotonergic antidepressants before psilocybin dosing. Any change in psychiatric medication should be done under the direct supervision of the prescribing clinician. Stopping antidepressants on your own risk withdrawal and relapse.
Final thoughts and guiding principles
Psilocybin is a powerful neurobiological tool: it can initiate profound, rapid plasticity and create the conditions for behavioral and psychological change. Its strongest evidence today is in treatment-resistant depression and in reducing existential distress in life-limiting illness, with promising early results for addiction. But it is not a magic bullet that works the same for everyone, nor is it risk-free.
If you or someone you know is contemplating psilocybin therapy, the safest path is through regulated clinical trials or licensed treatment programs that provide medical screening, trained guides, robust preparatory counseling, and structured integration. If you are exploring complementary supplements and lifestyle actions to support plasticity, adopt evidence-based foundational supports: adequate Vitamin D guided by blood testing, omega-3s at therapeutic dosages, nightly magnesium to support sleep, and consistent exercise and sleep hygiene. You can find a curated bundle of these essentials here. Avoid supplements that directly alter serotonin prior to or in the immediate peri-session window unless a physician clears them.