Today we’re taking a closer look at one of the most common medications in the health conversation right now: Ozempic, and similar GLP-1 drugs. These medications can be powerful tools for managing weight and metabolic health, but they often come with side effects that deserve attention. From hair loss and nutrient deficiencies to digestive changes, it’s important to understand not only what these side effects are, but also how to address them in practical, effective ways. In this post, we’ll break down the science behind the most common issues people experience, and share evidence-based strategies including targeted vitamin and supplement recommendations that may help reduce risks and support overall wellbeing. The goal is to give you clear, actionable guidance you can bring to your healthcare provider, so you feel more confident and informed in your treatment journey.
Table of Contents
- What these drugs are and how they work
- Common side effects — what to expect early and later
- “Ozempic face”: what it is and why it happens
- Hair loss after rapid weight loss — why it happens and how long it lasts
- Pancreatitis risk — what you need to know
- Thyroid tumor risk — animal data and human implications
- Kidney disease and cardiovascular effects — benefits and caveats
- Practical day-to-day tips while on these drugs
- Exact supplement protocol I discuss with patients
- Who should avoid these drugs
- Cosmetic use versus medical indications — ethical and practical points
- What to do if you experience adverse symptoms
- Long-term outlook and reversibility
- Frequently asked questions (FAQ)
- Closing thoughts
What these drugs are and how they work
Ozempic and Wegovy are branded formulations of semaglutide. Mounjaro (tirzepatide) and Zepbound are medications in the same broader family of injectable drugs used for diabetes and weight loss. Collectively, many of them are called GLP-1 receptor agonists (glucagon-like peptide 1 agonists) though tirzepatide is a dual GIP/GLP-1 receptor agonist, which is a slightly different mechanism but similar clinical effect: appetite suppression, slower gastric emptying, improved blood sugar control, and often significant weight loss.
These medications were developed to treat type 2 diabetes but doctors and patients noticed a prominent side effect: substantial weight loss in many patients. For some, that weight loss is life-changing. For others, it brings unexpected and sometimes distressing cosmetic effects like what’s become known in popular conversation as Ozempic face.
Common side effects — what to expect early and later
The most common side effects are digestive. Nausea, vomiting, diarrhea, and constipation are what patients report most frequently. For more on gastrointestinal side effects, see the Harvard Health overview of GLP-1 drug risks. These drugs are typically injected once weekly, and many people notice side effects within the first one to two days after an injection. For many patients these symptoms improve over the week as the dose is tolerated, and clinicians often titrate the dose gradually to reduce early intolerance.
- Onset: usually within 1–2 days after injection
- Trajectory: symptoms commonly ease over the following days
- Management: dose titration, anti-nausea strategies, and dietary adjustments
As the medication dose increases, side effects can increase too. That’s a predictable tradeoff: higher doses usually lead to more appetite suppression and more weight loss, but also more gastrointestinal symptoms.
“Ozempic face”: what it is and why it happens
When people talk about Ozempic face they mean the visible changes to the face that occur after relatively rapid weight loss: sunken cheeks, loss of midface fullness, more prominent cheekbones, and sometimes looser or sagging skin where there used to be fullness. I want to be clear: Ozempic doesn’t selectively remove fat from your face as if the drug knows where to target. What happens is more straightforward — when you lose a significant amount of weight, particularly in a short period of time, the fat under the skin shrinks. The face is one of the places where fat loss is noticeable early because facial fat is relatively superficial and contributes a lot to our perception of youth and fullness.

How pronounced the change is depends on:
- How much weight you lose and how fast you lose it
- Your age — older skin is less elastic and more likely to sag
- Your genetics — everyone has different fat distribution and skin elasticity
- Baseline facial fullness — if you had more facial fat to begin with, the change may be more apparent
For many people the facial changes are temporary as skin readapts; for others, especially older adults or people with significant weight loss, the change can be longer-lasting and might prompt consideration of aesthetic options like fillers, fat grafting, or surgical skin tightening. Those are personal decisions, and they don’t speak to the medical benefits many patients derive from these drugs.
Hair loss after rapid weight loss — why it happens and how long it lasts
Hair loss following substantial weight loss is well-documented and a common concern. Rapid weight loss can cause a type of hair shedding called telogen effluvium, where a large number of hair follicles prematurely enter the resting phase and fall out weeks to months after the triggering event.
The triggers in this setting are typically:
- Rapid reduction of caloric intake and temporary nutrient deficits
- Altered protein intake — hair is made of protein, and inadequate protein can precipitate shedding
- Physiologic stress associated with rapid body changes
Most of the time, telogen effluvium is reversible — hair starts to regrow once the underlying trigger is corrected. That said, regrowth can take months. While you’re waiting, there are nutritional and supportive steps you can take that may speed recovery or minimize the amount of shedding.

Nutrition and supplement strategies for hair support
Below I provide a set of supplements and dosages that I discuss with patients and that many clinicians and nutritionists recommend. These are meant as a starting framework to discuss with your physician. If you have kidney disease, thyroid disease, or another chronic condition, the exact treatment plan will change and some supplements may be contraindicated.
- Protein: Aim for 1.0 to 1.6 grams of protein per kilogram of ideal body weight per day for most adults when losing weight rapidly. If you’re very active or older, lean toward 1.2 to 1.6 g/kg. Example: if your ideal body weight is 70 kg, aim for 84 to 112 grams of protein per day. Consider 20–30 grams of high-quality protein (whey, egg, or plant-based concentrate) at each meal. If kidney disease is present, discuss lower targets with your nephrologist.
- Collagen peptides: 10 grams daily can be taken mixed in drinks. Collagen supplies amino acids useful for skin and hair matrix. It’s not magic, but it’s supportive.
- Biotin (Vitamin B7): 2,500 micrograms (2.5 mg) once daily. Many over-the-counter hair supplements use 2,500 to 5,000 mcg. Biotin deficiency is rare, but some people report less shedding with supplementation. High-dose biotin can interfere with certain lab tests, so tell your clinician if you take it.
- Zinc: 15 to 30 mg elemental zinc once daily for a limited course (8–12 weeks). Zinc deficiency can contribute to hair loss, but excessive zinc can cause copper deficiency, so avoid long-term high-dose use without monitoring.
- Iron: Only supplement if you are iron deficient. For premenopausal women, iron deficiency is common. Typical replacement doses are 45–65 mg elemental iron daily when treating deficiency — but do not begin iron without testing (ferritin and transferrin saturation). Iron supplementation without deficiency is not helpful and can be harmful.
- Vitamin D3: 1,000 to 2,000 IU daily as a maintenance dose is reasonable for most adults. If you are deficient (25-hydroxyvitamin D <20 ng/mL), higher repletion doses guided by a clinician (e.g., 50,000 IU weekly for 6–8 weeks) may be needed, then move to maintenance dosing. Vitamin D influences many body processes and deficiency can worsen overall recovery. Learn more about why optimal vitamin D levels are critical in this guide to vitamin D.
- Vitamin B12: 500 to 1,000 micrograms (mcg) daily oral sublingual or 1,000 mcg weekly sublingual or intramuscular if deficient. Particularly important for people reducing meat intake rapidly or people with absorption issues.
- Omega-3 (EPA/DHA): 1,000 mg combined EPA+DHA daily for general anti-inflammatory support. Higher doses (2–4 g) may be used under medical supervision for significant inflammation.
- Multivitamin: A once-daily multivitamin that provides 100% of the RDA for most vitamins and minerals is a sensible safety net during rapid weight loss.
For a curated supplement bundle that includes Magnesium, Vitamin D3 & K2, Hydrogen pills, and Omega-3, see the BetterLifeProtocols VIP pack.
These strategies focus on preventing or reversing nutritional contributors to telogen effluvium. I recommend a baseline panel before starting supplementation: CBC, ferritin, TSH and free T4, vitamin D (25-OH), B12, CMP (comprehensive metabolic panel) to evaluate kidney function, and if indicated, iron studies. That lets you target the supplements to real deficits.
Topical and systemic agents for hair loss
For people with persistent or severe shedding, some clinicians use medications or topical agents. Two common, evidence-supported options:
- Topical minoxidil: 2% solution twice daily, or 5% foam once daily (as tolerated). Minoxidil can help speed regrowth and is generally safe. Expect 3–6 months before seeing benefit.
- Prescription therapies: In specific cases, dermatologists may consider oral or topical options, hormonal evaluation, or other targeted therapies. If you have alopecia areata or another autoimmune hair loss condition, the approach differs significantly.
Important: avoid random high-dose supplements not supported by labs. For example, indiscriminate iron or very high-dose zinc can cause harm. Work with your clinician to target therapy.
Pancreatitis risk — what you need to know
There have been reports of pancreatitis in people taking GLP-1 agonists. In many analyses and large studies, a clear causal link has not been definitively proven. A comprehensive review of pancreatitis risk with GLP-1 agonists explores these data in more detail. The absolute risk appears small, but it is a real concern and something to be aware of. If you have a history of chronic pancreatitis or recurrent gallstone pancreatitis, your clinician will weigh that history carefully when recommending these drugs.
Practical guidance:
- If you have a prior history of pancreatitis, discuss alternatives with your provider; many clinicians will avoid GLP-1 receptor agonists in this group.
- If you develop unexplained abdominal pain while on the medication, have it evaluated promptly. Persistent or severe pain should trigger immediate medical attention, and temporary discontinuation of the medication is reasonable while pancreatitis is being ruled out.
- Serum lipase or amylase can help evaluate, but the clinical picture and imaging often guide management.
Thyroid tumor risk — animal data and human implications

One specific thyroid cancer called medullary thyroid carcinoma (MTC) showed an increased incidence in animal studies involving GLP-1 agonists. Because of that signal, drug labels often carry warnings. This is important to interpret correctly:
- The animal studies used high doses and species that have different thyroid physiology than humans.
- Human data have not conclusively demonstrated a significantly increased incidence of medullary thyroid carcinoma attributable to these drugs, but data continue to be collected.
- Because of the animal signal, regulatory agencies and manufacturers recommend that people with a personal or family history of medullary thyroid carcinoma or multiple endocrine neoplasia type 2 (MEN2) avoid these medications.
That is a clear clinical contraindication: if you or a close family member has MTC or MEN2, do not take GLP-1 receptor agonists without specialized input. A meta-analysis of randomized trials suggests the absolute risk of pancreatitis is low and no definitive increase has been demonstrated in controlled settings.
Kidney disease and cardiovascular effects — benefits and caveats
While we’re focused on side effects, it’s vital to remember these drugs have pronounced benefits for many patients. For people with type 2 diabetes, they improve glycemic control. There’s evidence that in diabetic patients GLP-1 receptor agonists can slow progression of diabetic kidney disease and reduce certain cardiovascular risks. These are not trivial effects, they’re part of why these drugs were widely adopted in the diabetic population even before the current focus on weight loss.
At the same time, kidney disease modifies how I approach supplemental recommendations. Aggressive protein intake can be harmful in advanced kidney disease. Some supplements that are otherwise safe can accumulate in renal failure (for example, magnesium or certain herbal preparations). That’s why I underscore again: if you have chronic kidney disease, coordinate any supplement plan with your nephrology team.
Practical day-to-day tips while on these drugs
Here are practical strategies I recommend for patients taking GLP-1 receptor agonists to reduce side effects and preserve nutrition and quality of life.
Start slow and titrate
Follow your prescriber’s titration schedule closely. Most of the nausea and GI upset occurs early and improves as your body adapts. Slower titration often means fewer side effects and better long-term adherence.
Small, frequent, protein-focused meals
Because appetite is suppressed and caloric intake drops, focus on protein at every meal. Protein helps preserve lean mass and supplies the amino acids needed for hair and skin health. Try to have a protein source at each eating opportunity — dairy, eggs, fish, poultry, legumes, or a protein shake when whole-food meals aren’t possible.
Hydration and electrolytes
Diarrhea or vomiting can lead to dehydration and electrolyte losses. Not all magnesium supplements are equal — see this breakdown on different forms of magnesium. Drink water steadily. If you have persistent diarrhea, a sports drink or an oral rehydration solution for short periods can help replace sodium and potassium. If you’re on blood pressure medications or diuretics, monitor closely because weight loss and changes in intake can change blood pressure.
Avoid unproven or risky herbal supplements
Many “hair growth” or “detox” supplements contain high doses of ingredients that can interfere with medications or cause GI distress. Stick to clinically validated nutrients like zinc, iron when deficient, vitamin D, B12, omega-3, and a good quality protein supplement.
Regular lab checks
Before and during therapy, baseline labs and periodic monitoring are prudent: CBC, CMP (including creatinine), liver function tests, fasting glucose/HbA1c as indicated, thyroid testing if symptomatic or family history, ferritin and iron studies if hair loss occurs, and vitamin D/B12 if deficiency is suspected.
Exact supplement protocol I discuss with patients
Below is a consolidated protocol I use as a starting point when patients tell me they’re taking a GLP-1 agonist and want to minimize hair loss and nutrient issues. This is an educational framework; do not start everything here blindly. Bring it to your clinician, get baseline labs, and tailor it to your needs.
- Baseline labs (before or soon after starting the drug)
- CBC with differential
- Ferritin and iron studies
- Comprehensive metabolic panel (including creatinine)
- Thyroid-stimulating hormone (TSH) and free T4
- Vitamin D 25-hydroxy
- Vitamin B12
- Optional: lipid panel, HbA1c (if diabetic or prediabetic)
- Daily nutrition and supplement starter pack
- High-quality protein intake: 1.0–1.6 g/kg ideal body weight per day. Use whole foods and consider protein shakes (20–30 g per serving) if needed.
- Collagen peptides: 10 g once daily mixed into coffee or smoothie.
- Biotin: 2,500 mcg (2.5 mg) once daily.
- Vitamin D3: 2,000 IU once daily (adjust if labs show deficiency).
- Vitamin B12: 500–1,000 mcg daily oral sublingual or 1,000 mcg weekly if starting parenteral therapy is not needed.
- Zinc: 15–30 mg elemental zinc once daily for 8–12 weeks; monitor and do not continue high doses long-term without testing for copper.
- Omega-3 (fish oil): 1,000 mg combined EPA/DHA once daily.
- Multivitamin: once daily to cover other micronutrients.
- Targeted therapy if labs show deficiencies
- Iron deficiency: Treat with oral iron providing 45–65 mg elemental iron daily (or as prescribed) until ferritin and iron studies normalize. Recheck ferritin after 8–12 weeks.
- Vitamin D deficiency: Repletion protocols (e.g., 50,000 IU weekly for 6–8 weeks) followed by 1,000–2,000 IU maintenance, guided by labs.
- Vitamin B12 deficiency: 1,000 mcg intramuscular weekly for 4–6 weeks or high-dose oral/sub-lingual 1,000 mcg daily until stable, then maintenance dosing.
- Topical and prescription hair aids
- Topical minoxidil 5% foam once daily or 2% solution twice daily for at least 3–6 months before judging effect.
- If autoimmune or patterned hair loss is suspected, referral to a dermatologist is appropriate.
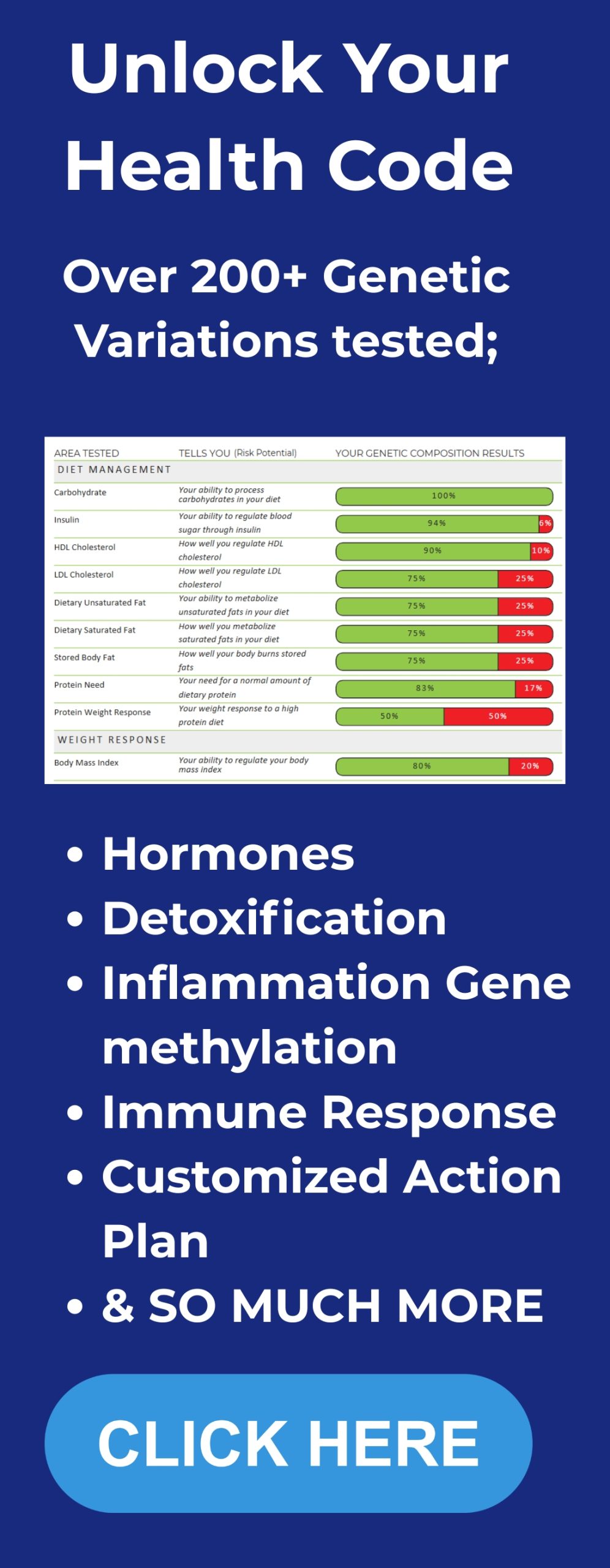
For deeper personalization, DNA testing can reveal nutrient needs and metabolic tendencies — explore BetterLifeProtocols DNA insights.
Again, these are starting points. If you have chronic kidney disease, we will lower protein targets and scrutinize every supplement. If you have thyroid cancer risk in your personal or family history, avoid GLP-1 agents unless a specialist advises otherwise.
Who should avoid these drugs
These medications have transformed care for many patients, but they are not right for everyone. Key contraindications or strong cautions include:
- Personal or family history of medullary thyroid carcinoma or MEN2
- Pregnancy or planning pregnancy — weight loss drugs are not appropriate during pregnancy
- Active or recent pancreatitis in some cases — discuss with your provider
- Significant gastrointestinal disease that would be worsened by delayed gastric emptying or severe nausea
Outside of these groups, many people are eligible for consideration; the decision should be individualized based on benefits versus risks.
Cosmetic use versus medical indications — ethical and practical points
There’s public debate about people using these medications for cosmetic weight loss, and that’s a legitimate societal conversation. From a medical perspective, these drugs have important benefits for people with obesity-related health problems and for patients with type 2 diabetes who face cardiovascular and kidney risks. For patients using them purely for cosmetic reasons, prescribers reasonably weigh risks, potential side effects, and drug access concerns. My view is balanced: these medications have a strong medical role, but they also carry real side effects and risks that should inform any decision to start them.
What to do if you experience adverse symptoms
Practical steps if you develop symptoms while taking a GLP-1 agonist:
- Persistent vomiting, severe or worsening abdominal pain, or signs of dehydration: seek urgent medical attention; pancreatitis must be ruled out.
- New or worsening thyroid-related symptoms such as a rapidly growing neck mass, hoarseness, or difficulty breathing: contact your provider for evaluation.
- Significant hair loss: get labs (CBC, ferritin, TSH, vitamin D, B12) and consider initiating the nutritional protocol above while awaiting results.
- If GI side effects are limiting: discuss dose reduction or slower titration and symptomatic medications with your prescriber.
Long-term outlook and reversibility
Many side effects are reversible. Hair loss from telogen effluvium usually recovers over months once nutrition and physiologic stressors are corrected. Weight-loss related facial changes may partially reverse if weight stabilizes and skin elasticity allows, but some people choose cosmetic procedures for more immediate or dramatic changes.
Pancreatitis and medullary thyroid carcinoma are serious but relatively rare events; vigilance and appropriate screening/history-taking minimize surprises. For many patients, the metabolic benefits which are improved blood glucose control, slowed progression of kidney disease in diabetics, and reduced cardiovascular events, outweigh the risks, but the decision must be individualized.
Frequently asked questions (FAQ)
Q: Will everyone on Ozempic get Ozempic face?
A: No. The degree of facial change is highly individual. People who lose a lot of weight quickly are more likely to notice facial fat loss. Age, skin elasticity, genetics, and baseline facial fullness play major roles. Not everyone will experience dramatic facial changes, but it is a common enough phenomenon that it’s worth discussing before you start therapy.
Q: If I lose hair while taking a GLP-1 drug, is it permanent?
A: Usually not. Most post-weight-loss hair shedding is telogen effluvium, which is temporary and typically reversible over months once nutrition and metabolic stressors are addressed. However, if hair loss is sudden, patchy, or associated with other concerning signs, see a dermatologist to rule out other causes.
Q: Can I prevent hair loss entirely?
A: You can reduce risk and severity by proactively addressing nutrition: sufficient protein, correcting iron and vitamin deficiencies, ensuring adequate vitamin D and B12, and using targeted supplements like biotin and zinc when appropriate. Topical minoxidil can help support regrowth. Prevention is not guaranteed but these steps give you the best chance.
Q: Are the thyroid cancer warnings based on human data?
A: The strongest signal came from animal studies. Human data have not definitively proven a causal relationship for medullary thyroid carcinoma, but because of the animal signal, the precaution is real: people with a personal or family history of medullary thyroid carcinoma or MEN2 should not take these drugs.
Q: Do these drugs cause pancreatitis often?
A: No. Pancreatitis reports exist, but the absolute risk appears small. If you have a history of pancreatitis, this may influence the decision to use these drugs. Any unexplained persistent abdominal pain while on the medication should prompt evaluation for pancreatitis.
Q: What about kidney disease?
A: For many diabetic patients, GLP-1 receptor agonists have been shown to slow kidney disease progression. However, if you already have advanced kidney disease, supplemental and protein recommendations change. Work closely with your nephrologist.
Q: What should I tell my clinician before starting one of these drugs?
A: Give a full medical and family history, especially regarding pancreatitis, thyroid cancers, and kidney disease. Discuss your goals for weight loss and your threshold for side effects. Ask for a baseline panel where appropriate (CBC, CMP, ferritin, TSH, vitamin D, B12) so you have a roadmap to prevent and treat deficiencies.
Closing thoughts
These medications are powerful tools with real metabolic benefits for many people. They are not magic bullets, and they come with tradeoffs. My goal in this article is to translate the clear clinical insights from the Northwell Health presentation into practical, actionable steps you can use right now to prevent or mitigate the most common side effects, particularly hair loss and nutrition-related problems. Use the supplement dosages and lab guidance here as a starting point for a conversation with your clinician.
If you’re ready to put these strategies into action, check out our Integrate protocols that you put into daily life.