Introduction: Why your mood is as much about your gut as your head
Emotions are not just something that happen inside your skull. They are the product of an ongoing conversation between your brain and your body. Today, I want to walk you through how food, nutrients, and even your beliefs about food shape how you feel. I’ll explain concrete biology so you understand why certain meals make you feel wired, flat, calm, or energized. Then I’ll share exact, practical protocols for supplements, dosages, and daily behaviors you can use to shift your mood in reliable ways.
This is not theoretical. The gut contains specialized sensors, neurons, and communities of microbes that constantly send information to your brain. That information biases neural circuits toward pursuit, avoidance, calm, or arousal. Foods deliver amino acids and fats that are the raw materials for the brain chemicals that govern motivation and well-being. And your beliefs about a food can change the physiology of hunger and satiety in measurable ways.
Attraction versus aversion: the simplest model of emotion

At its core, emotions are about action. We lean in toward what’s attractive and away from what’s aversive. That tendency is ancient and obvious when it comes to taste and smell. Attractive cues prompt you to inhale and orient your body toward the source. Aversive cues produce recoil, nausea, cringing, or avoidance. Those reactions likely evolved to help organisms ingest nutrient-rich substances and avoid toxins.
From a neuroscience perspective, brain circuits that promote movement and action (go circuits) and circuits that suppress action (no go circuits) are engaged by these attractive and aversive signals. Emotions emerge from the interplay between these circuits and continuous input from the body. That’s why feeling is embodied: your gut, heart, lungs, and immune signals all bias which circuits are active.
Why this matters for daily life
If we understand emotions as action biases shaped by bodily signals, it becomes clear that changing the inputs to your body, what you eat, how you breathe, how you move, changes how your brain interprets the world and what you do next. That is enormously empowering because it means there are practical things you can do to shift mood, craving, and motivation.
The vagus nerve: the body’s sensory superhighway
The vagus nerve is the 10th cranial nerve. Think of it like the sensory wiring of your body’s interior. One branch connects to the brainstem while other branches innervate the stomach, intestines, heart, lungs, and elements of the immune system. The vagus is to the gut what the optic nerve is to the eyes: a continuous stream of information about the internal environment.
Vagal inputs include the presence of sugars, fats, amino acids, degrees of stretch in the stomach, inflammatory signals, and more. Those inputs pass through brainstem stations and influence neuromodulatory systems like dopamine and serotonin. That means your gut is constantly updating the brain about whether to pursue or avoid, rest or move.
Sugar sensing in the gut: hidden sugars drive craving

We tend to think taste drives eating behavior. Taste matters, but taste is only part of the story. The gut has sugar-sensing cells that detect sugars independent of whether your tongue perceives sweetness. Those gut sensors signal up via the vagus nerve to reward circuitry and trigger dopamine release. That dopamine release increases desire and makes you want more of what you just ingested.
Here’s the startling practical implication: foods that contain hidden sugars like salad dressings, sauces, commercial breads, and processed savory foods can trigger craving even if you cannot taste the sugar. Experiments have shown that when taste and visual cues are removed, people still prefer and consume more of foods that contain sugar because gut sensors are detecting sugar and driving reward signals.
How to use this knowledge
- Audit processed foods for added sugars even when the food tastes savory.
- When trying to reduce cravings, prioritize whole foods with minimal added sugars. Read labels for syrups, maltodextrin, cane sugar, fructose, and other hidden sweeteners.
- Understand that a craving may be gut-driven and not simply a failure of willpower.
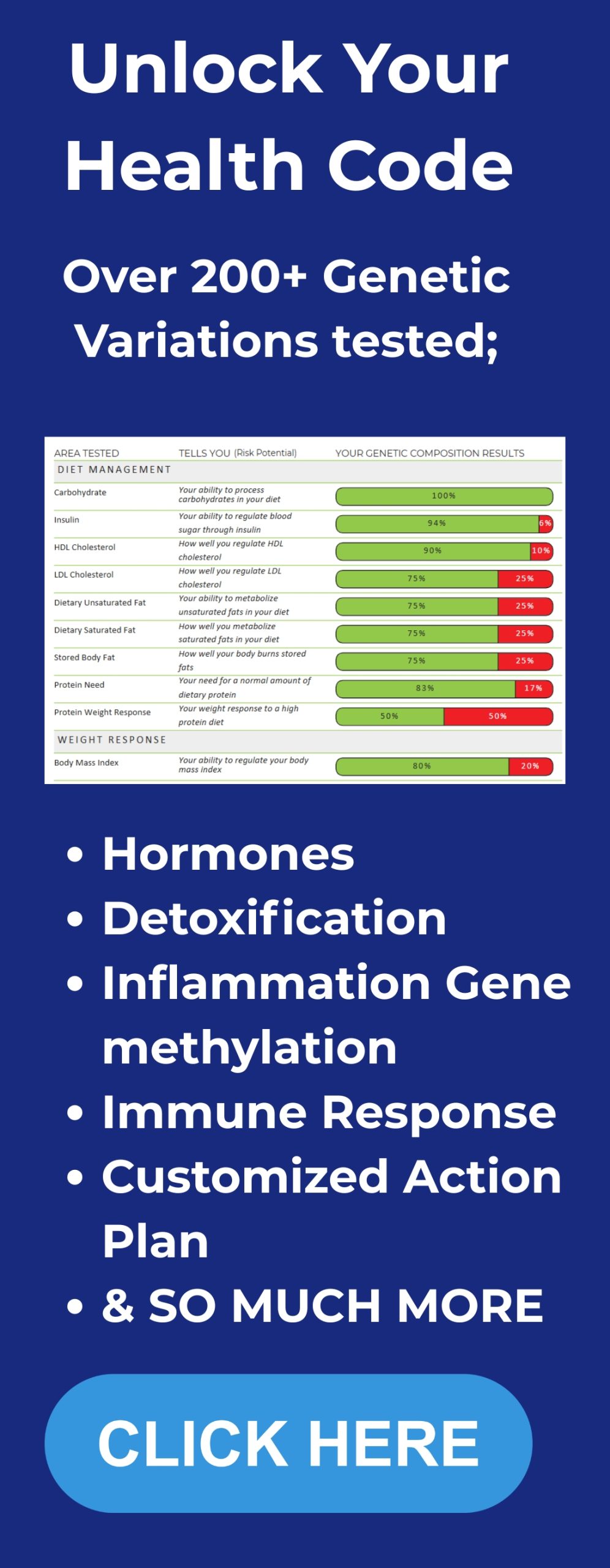
Amino acids, L-tyrosine, and dopamine: the chemistry of wanting
Amino acids are the building blocks of neurotransmitters. Dopamine is synthesized from the amino acid L-tyrosine. When your gut signals adequate availability of certain amino acids, the brain receives feedback about nutrient sufficiency and motivation states shift.
Shop now: Organika Glycine – Amino Acid
Dopamine is less about pleasure and more about craving, motivation, and pursuit. When expectation and outcome align or exceed one another, dopamine increases and you are motivated to pursue that object or action again. When outcomes fall short of expectation, dopamine drops and you’re less likely to pursue. That reward prediction error mechanism underlies addiction, habit formation, and food choice.
When supplementation makes sense: L-tyrosine
Some people have low dopamine synthesis or function. In clinical settings, Parkinson’s disease is treated with L-dopa because dopamine neurons are degenerated. Most people do not need prescription L-dopa, but some benefit from L-tyrosine supplementation or simply increasing dietary protein because it provides the amino acid precursors for dopamine.
Practical dosing and cautions I use and recommend for general-purpose L-tyrosine supplementation:
- Starter dose: 500 mg in the morning on an empty stomach to test tolerance.
- Effective range for many people: 500 mg to 1,500 mg taken in the morning. Do not exceed 2,000 mg per day without medical supervision.
- Avoid taking L-tyrosine late in the day because it can increase alertness and potentially disturb sleep.
- People with bipolar disorder or mania should not take L-tyrosine without consulting a psychiatrist because elevating dopamine may worsen manic symptoms.
- There can be a rebound crash in energy and mood after acute use. If you feel lethargic or foggy the day after supplementation, reduce dose or discontinue.
Food-first approach: include high-quality protein sources at breakfast such as eggs, lean meats, or soy products to naturally supply L-tyrosine and other catecholamine precursors.
Serotonin and carbohydrates: using food to promote calm and sleep
Serotonin is a neuromodulator that biases which circuits are active. Elevated serotonin creates a sense of comfort and contentment. In contrast to dopamine and epinephrine, which support pursuit and arousal, serotonin supports rest, digestion, and social ease.
Most serotonin in the body exists in the gut, but the serotonin that influences mood and cognitive state is synthesized by neurons in the brainstem, specifically the raphe nuclei. That neuronally produced serotonin depends on the availability of its precursor, tryptophan, an essential amino acid.
Carbohydrates and serotonin synthesis
Carbohydrate intake can increase the relative availability of tryptophan to the brain, thus promoting serotonin synthesis. That is one reason carbohydrate-rich meals tend to produce a calming, sometimes sleepy effect. People often exploit this by favoring higher-carb snacks in the evening to promote sleep.
My practical approach for daily timing:
- Morning and mid-day: emphasize protein and moderate fat with low to moderate carbohydrates to favor dopamine, acetylcholine, and alertness. For example, a high-protein breakfast with vegetables and healthy fats.
- Evening: favor a modest carbohydrate-rich component with tryptophan-containing foods to support serotonin and sleep. Foods include oats, rice, turkey, dairy, bananas, and nuts.
If you already take antidepressants such as selective serotonin reuptake inhibitors SSRI, be cautious about adding serotonin-boosting supplements without medical advice. Foods are generally safe, but combining pharmacological and herbal or supplemental serotonin precursors can cause adverse effects.
Omega-3 versus omega-6 fatty acids: ratio matters for depression
Inflammation and membrane composition in neurons are influenced by the balance of omega-3 and omega-6 polyunsaturated fatty acids. Many contemporary diets are excessive in omega-6s and deficient in omega-3s, and that shift can affect mood and inflammatory signaling.
One striking set of findings compared 1,000 mg of pure EPA (eicosapentaenoic acid, an omega-3 component) to 20 mg of fluoxetine, a common SSRI. In that study, EPA at 1,000 mg per day reduced depressive symptoms to an extent similar to 20 mg fluoxetine. The combination of EPA and fluoxetine produced an additive or synergistic effect in reducing symptoms.
Practical omega-3 guidance
- Aim for at least 1,000 mg of EPA per day when addressing mood support. Many effective omega-3 supplements provide a combined EPA and DHA total in capsules; check the label to ensure EPA content.
- If you cannot tolerate fish oil, consider high-EPA formulations or talk with a clinician about prescription omega-3 options.
- Dietary sources: fatty fish such as salmon, mackerel, sardines, and anchovies provide EPA and DHA. Aim for two servings of fatty fish per week as a baseline food target.
- Balance omega-6 intake by reducing excessive vegetable oils high in linoleic acid and processed foods rich in seed oils.
- Discuss with your doctor before starting omega-3 supplements if you are on blood thinners or have a bleeding disorder because high-dose omega-3s can affect clotting.
Gut microbiome: why it is not simply good or bad and how to influence it

The gut microbiome refers to the collection of microorganisms living along the digestive tract. They are not sentient helpers. They are opportunistic. Their survival depends on them shaping the mucosal environment which include its pH, mucus, and nutrient availability, to favor their replication.
Some microbes improve digestive efficiency, bolster immune function, and positively influence neurotransmitters. Others can promote inflammation, produce metabolites that impair mood and cognition, and encourage states that feel unwell. Thus the microbiome is context dependent and individualized.
Fermented foods, probiotics, and prebiotics
Fermented foods are among the most effective and low-risk ways to support a healthy microbiome. Foods such as yogurt with live cultures, kefir, kimchi, sauerkraut, kombucha, and miso supply live microbes and create favorable environments without the extremely high doses you find in supplements.
Recommendations I use and share:
- Aim for at least two servings of fermented foods per day. A serving could be 100 grams of yogurt, 1 cup of kefir, or a small bowl of sauerkraut or kimchi. Two servings per day supports microbial diversity without overshooting.
- Probiotic supplements can be beneficial but do not assume more is better. Typical low-to-moderate supplement doses range from 1 billion to 10 billion CFU per day for maintenance. Some therapeutic protocols use higher doses, but very high and indiscriminate dosing of certain strains such as Lactobacillus can cause brain fog, bloating, or digestive discomfort in some people.
- Prebiotic fibers, such as inulin, resistant starch, and certain oligosaccharides, feed beneficial microbes. Introduce prebiotics slowly to avoid gastrointestinal discomfort and start with low doses, 2 to 5 grams per day, increasing as tolerated.
- Target diverse plant fiber sources: aim for a variety of vegetables, fruits, whole grains (if tolerated), nuts, seeds, and legumes to provide substrates for a diverse microbiome.
- Avoid excessive use of antibiotics unless clearly medically necessary. When antibiotics are used, pair recovery strategies including fermented foods and appropriate probiotic regimens under clinical guidance.
Artificial sweeteners and the microbiome
Not all artificial sweeteners affect the microbiome the same way. Research shows that saccharin in particular has the capacity to shift the microbiome in ways that increase inflammation and impair metabolic markers in some individuals. Other common sweeteners such as aspartame, sucralose, and stevia have more mixed data and do not uniformly produce the same negative shifts as saccharin in published studies.
Actionable takeaways:
- Avoid saccharin-containing products when possible.
- If you use non-nutritive sweeteners, assess how you feel and consider rotating or reducing usage if you experience digestive discomfort, inflammation, or worsening mood.
- Prioritize whole-food sweeteners like modest amounts of honey or maple when you need sweetness, and understand these still provide sugars and can drive gut sugar-sensing and craving.
Diet is personal: find the microbiome and nutrition plan that fits you
People respond differently to diets such as ketogenic, plant-based, vegetarian, or omnivorous. Changing diet profoundly alters the microbiome and some people feel dramatically better after switching. Others feel worse. Genetic makeup, early-life exposures, and the preexisting microbiome all influence how a diet change will feel.
My recommendation: experiment systematically and keep a symptom and mood log. When trying a new diet, try it for at least two to four weeks while tracking sleep, mood, digestion, energy, and cognitive clarity. Make one change at a time so you can attribute effects to the change.
To understand your individual genetic tendencies for nutrient metabolism and mood regulation, explore our personalized DNA insights program.
Belief and physiology: the milkshake and grelin study
Mindset matters. A medical team ran an elegant experiment where two groups consumed identical milkshakes. One group was told the shake was a low-calorie health shake. The other was told the shake was a decadent high-calorie indulgence. Blood samples measured ghrelin, the hunger hormone.
Results: the group told they had consumed a high-calorie shake experienced a stronger suppression of ghrelin than the group told they consumed a low-calorie shake. Belief about the food altered peripheral physiology. This is not simple self-deception. For belief effects to work you typically need to be genuinely naive to the manipulation. You cannot merely lie to yourself and expect the same physiological effect.
Practical applications of mindset effects
- When you plan meals, frame them positively. If you expect a meal to be nourishing and satisfying, your body will often respond differently than if you anticipate deprivation.
- Use intentional labeling: when preparing a nourishing evening meal, take a moment to note that the meal is supportive of sleep and recovery. This simple cognitive step may enhance digestive and hormonal responses.
- Avoid constant dieting mindsets that emphasize restriction; chronic dieting signals scarcity and can dysregulate hunger hormones and mood over time.
Actionable daily protocol: what I personally recommend
Below is a pragmatic, food-first protocol that I use with people and personally adapt and it forms the foundation of our Integrate Program for long-term mood and metabolic balance. It addresses morning alertness, daytime performance, craving control, mood stabilization, microbiome support, and evening recovery for sleep. It includes exact supplement suggestions and doses where I believe evidence supports them, along with safety cautions.
Morning routine
- Wake with natural light exposure within 30 minutes of waking for 10 20 minutes to set circadian rhythms.
- Hydrate with 300 500 milliliters of water. Add a pinch of salt if you feel lightheaded or have low blood pressure.
- Breakfast: high protein, moderate fat, low carbohydrate to favor dopamine and alertness. Example: 2 eggs, sautéed spinach, half an avocado, and a small serving of berries. This supplies L-tyrosine and other amino acids without a heavy carb load that would drive serotonin early in the day.
- L-tyrosine supplementation (optional): start with 500 milligrams in the morning taken at least 30 minutes before breakfast if you want to test alertness enhancement. Increase cautiously to a maximum of 2,000 milligrams per day only under medical supervision. Do not use if you have predisposition to mania.
Midday and afternoon
- Lunch: maintain moderate protein and vegetables. If you need alertness for work, keep carbohydrates lower and favor complex carbs if required.
- Omega-3 supplementation: take fish oil that provides at least 1,000 milligrams EPA daily. If your supplement lists combined EPA+DHA, verify EPA is at or near 1,000 milligrams or choose a high-EPA formula. For general health, combined 1,000 to 2,000 milligrams of EPA+DHA daily is common; for mood-focused protocols prioritize EPA content.
- Movement break: a 20-minute walk or short resistance set to assist glucose regulation and support microbiome diversity through increased gut motility.
Evening and sleep preparation
- Dinner: include a modest carbohydrate portion with tryptophan-rich foods to encourage serotonin and subsequent melatonin production. Examples: grilled salmon with a small portion of rice and steamed vegetables, or turkey with sweet potato and greens.
- Aim to finish heavy eating at least 2 to 3 hours before bed to reduce reflux and promote restorative sleep.
- If sleep initiation is a problem, consider foods high in tryptophan or a low dose of a sleep-support supplement only after consulting with a clinician. Avoid combining serotonin precursors with SSRIs unless medically cleared.
Microbiome daily practices
- Consume at least two servings of fermented foods per day: yogurt, kefir, kimchi, sauerkraut, or miso. These small, consistent servings support microbial diversity without the high-dose risks associated with some supplements.
- If using a probiotic supplement, start low. A practical starting dose is 1 to 10 billion CFU per day of a multi-strain formula. Monitor for brain fog, bloating, or changes in mood. Increase only if clearly beneficial under guidance.
- Include diverse plant fibers across meals. Aim for 25 to 40 grams of fiber per day from vegetables, fruit, nuts, and legumes as tolerated.
When to consider professional interventions
- If you are clinically depressed, have suicidal thoughts, or have severe functional impairment, seek professional psychiatric care. Supplements can be adjuncts but not replacements for appropriate clinical care.
- If you are taking prescription medications especially SSRIs or MAO inhibitors, always consult a prescriber before starting L-tyrosine, tryptophan, 5-HTP, or high-dose omega-3s.
- If you have a bleeding disorder or are on anticoagulants, consult before high-dose omega-3 supplementation.
Supplement cheat sheet with dosages and notes
Below are concise recommendations. Treat these as starting points to discuss with your primary care provider or a clinician who knows your medical history. I am sharing what I use and recommend at Betterlifeprotocols.com, but individual factors matter.
- EPA (omega-3): Aim for 1,000 mg EPA daily for mood support. If your fish oil provides combined EPA+DHA, verify EPA content. Typical combined dose for general health 1,000 2,000 mg total EPA+DHA.
- L-tyrosine: 500 mg morning starter dose. Effective range 500 1,500 mg in the morning. Max 2,000 mg without supervision. Avoid with mania or certain medical conditions.
- Fermented foods: Two servings per day. Example serving sizes: 100 150 grams yogurt, 1 cup kefir, 50 grams kimchi or sauerkraut.
- Probiotic supplements: Start 1 10 billion CFU per day of a broad-spectrum, multi-strain formula. Monitor for brain fog or adverse reactions; higher doses are not always better.
- Prebiotic fiber: Start 2 5 grams per day and build to 10 15 grams as tolerated.
- Tryptophan-rich evening foods: Include turkey, dairy, oats, rice, bananas, or nuts in evening meals. If using supplemental tryptophan or 5-HTP consult prescriber.
- Avoid saccharin-containing artificial sweeteners where possible, as evidence shows saccharin can shift microbiome composition negatively in some people.
Practical meal templates for a week
Below are simple meal templates that incorporate the principles above: morning protein emphasis, microbiome support, daytime focus, and evening serotonin support. Rotate ingredients to keep variety and nutrients diverse.
Day 1
- Breakfast: Omelette with spinach, mushrooms, and feta. Side 50 grams mixed berries.
- Snack: 1 small apple and a handful of almonds.
- Lunch: Grilled chicken salad with mixed greens, olive oil vinaigrette (no added sugars), and a small serving of quinoa.
- Fermented food: 150 grams plain Greek yogurt in afternoon.
- Dinner: Salmon with a small portion of brown rice, steamed broccoli, and kimchi side. Finish eating 2 3 hours before bed.
Day 2
- Breakfast: Plain kefir smoothie with spinach, half banana, and a scoop of whey or plant protein.
- Snack: Carrot sticks and hummus.
- Lunch: Beef stir-fry with vegetables and cauliflower rice.
- Fermented food: Small serving of sauerkraut with lunch or dinner.
- Dinner: Turkey chili with beans and a side of brown rice.
Repeat variations across the week, ensuring at least two servings of fermented foods every day and rotating fish meals to reach weekly omega-3 targets.
Tracking outcomes: simple metrics to notice improvements
When you change diet and supplements, track the following metrics for at least two to four weeks so you can evaluate whether changes are beneficial:
- Mood rating each morning on a 1 to 10 scale.
- Sleep quality and latency: how long it takes to fall asleep and how rested you feel.
- Energy and focus during the main work period of the day.
- Cravings: frequency and intensity of sugar or carb cravings.
- Digestive symptoms: bloating, bowel frequency, stool consistency.
FAQ
Can I take L-tyrosine every day to stay motivated?
You can try L-tyrosine as a short-term or occasional tool, but chronic daily high-dose L-tyrosine can disrupt dopamine pathways and cause rebound fatigue or brain fog. Start with 500 mg in the morning to assess tolerance. If helpful, many people maintain 500 to 1,500 mg on days when they need extra focus. Avoid long-term unsupervised use at high doses and consult a clinician if you have bipolar disorder, are on monoamine-affecting medications, or have other medical conditions.
How do I choose a fish oil supplement and what should the label show?
Look for third-party tested fish oil that specifies EPA and DHA amounts per serving. For mood support prioritize EPA. A practical target is 1,000 mg EPA daily. If the product gives combined EPA+DHA, check the EPA portion specifically. Choose molecularly distilled or purified products to reduce contaminants. If you are on blood thinners consult your prescriber before starting high-dose omega-3s.
Are fermented foods enough or do I need probiotic supplements?
Fermented foods are a safe, effective baseline and I recommend two servings per day. Probiotic supplements can be useful for specific conditions but are not always better than foods. Start low with supplements 1 to 10 billion CFU and monitor for side effects like brain fog or bloating. Some people do well with a combined approach; others do better with only fermented foods. Personalize based on outcomes.
Will carbohydrate-rich dinners make me gain weight?
Carbohydrate timing matters more for sleep and serotonin than for weight per se. If you control total daily caloric intake and macronutrient balance, a modest carbohydrate portion in the evening can help sleep without causing weight gain. Focus on whole-food carbohydrates like rice, oats, sweet potato, and avoid excess liquid calories and hidden sugars in processed foods.
How quickly can I expect to see mood benefits from these changes?
Some changes are fast: fermented foods and a single high-protein morning can shift alertness and cravings within days. Omega-3 benefits for mood often require several weeks of consistent dosing, commonly 4 to 12 weeks. Microbiome shifts can produce detectable changes in mood and digestion over weeks, but durable effects require consistent dietary patterns and lifestyle practices including sleep and exercise.
Is saccharin the only artificial sweetener to avoid?
Research has specifically implicated saccharin in deleterious shifts in the microbiome in some studies. Other sweeteners like aspartame, sucralose, and stevia show mixed results and may be better tolerated for many people. However, non-nutritive sweeteners can maintain sweet preferences and sometimes perpetuate cravings. Prefer whole-food sweetness and evaluate individual responses.
Can mindset changes really alter hunger hormones?
Yes. Experiments where participants consumed identical shakes but were told different calorie information produced different ghrelin responses. If you genuinely believe and are naive to the information, your physiology can respond differently. Use this by framing your meals as nourishing and restorative to enhance physiological satiety signals.
Wrapping up: practical next steps and safety reminders
Your mood is not a mystery separate from biology. Food, nutrients, and the microbial community in your gut combine with your beliefs and behaviors to create the day-to-day experience of contentment, drive, and calm. Use the actionable steps above: prioritize high-protein breakfasts, modest evening carbs for sleep, at least two servings of fermented foods daily, and consider a targeted omega-3 intervention of approximately 1,000 mg EPA daily for mood support.
Safety first: before beginning any supplement regimen, talk with your physician, especially if you take prescription medications, have a psychiatric history, are pregnant or nursing, or have chronic medical conditions. Supplements can be powerful adjuncts, but they are not substitutes for clinician-guided treatment when required.
Take one step this week: pick one habit from this guide to add (maybe two servings of fermented foods daily, or swapping hidden-sugar sauces for whole-food alternatives). Then, learn how to connect nutrition, mindset, and lifestyle using our Integrate Protocol for sustainable change. Track mood, sleep, and cravings for two weeks and see what changes. Small, consistent adjustments are where durable improvements in mood come from.