Today we’re diving into a topic that doesn’t get nearly enough honest discussion: what really happens to the body when someone loses a large amount of weight quickly. Inspired by the Netflix docu-series Fit for TV: The Reality of The Biggest Loser and insights from Dr. Robert Huizenga (known on the show as Dr. H), as well as former contestants, this conversation pulls back the curtain on the science, the recovery process, and the truth behind the media narrative.
In this post, we’ll explore what research actually shows about rapid weight loss, how the body responds, and why the story is often more complex than it appears on television. We’ll also highlight practical strategies for recovery and long-term maintenance—covering nutrition, supplements, exercise, and evidence-informed lifestyle choices. You’ll learn the potential risks, the areas where science is still uncertain, and the specific steps that can make a lasting difference. By the end, you’ll have a clearer understanding of how to approach weight loss in a way that supports both immediate results and long-term health.
Table of Contents
- Why this conversation matters
- What contestants say: Hannah’s experience
- The data the show produced and what it showed
- Did the show break people’s metabolisms? The NIH study controversy
- What went wrong with public perception
- Aftercare, responsibility and the reality of television
- What the science recommends for preserving metabolic health during large weight loss
- Specific exercise recommendations
- Nutrition and protein targets
- Vitamins, supplements and exact dosages I discuss with clinicians
- How to measure your metabolic rate accurately
- Practical, step by step maintenance plan after rapid weight loss
- What role should television producers and clinicians play
- How to talk to your clinician about large losses and maintenance
- Realistic expectations and personal stories
- Policy implications and the path forward
- Summary and takeaways
- FAQ
- Final thoughts
Why this conversation matters
Reality television created a set of images and expectations about weight loss that are hard to forget. The Biggest Loser turned dramatic, rapid weight loss into entertainment. The show also provided medical oversight, led by Dr. Huizenga, and collected a lot of clinical data over multiple seasons. What makes this story compelling and complicated is that the human outcomes diverged. Some contestants regained most of their weight. Some maintained major improvements. Many experienced psychological and medical challenges along the way.
What I wanted to know, and what I asked Dr. H directly, was simple: did the show cause lasting metabolic harm? Was the headline that contestants had permanently damaged metabolisms accurate? If not, why did people believe it, and what can we learn to protect people who choose aggressive weight loss pathways in the future?

What contestants say: Hannah's experience
Hannah, a former contestant who appears on the documentary, gave a powerful personal testimony that captures the complexity. She initially said she was humiliated when producers approached her, but she also credited the program for giving her critical mental health support, medical care, and education about diet and exercise.
“It wasn’t something that I really thought like I needed, but it was everything that I absolutely needed. I went on the show. I got the mental health help that I really needed. I met with a show psychologist, obviously Dr. Huizenga, Julian and Bob. And we really felt very supported throughout the whole entire journey.”
Hannah walked onto her season prediabetic and diagnosed with infertility. Since the show, she told me, she has two children and she reached and sustained a maintenance weight through the combination of what she learned on the show and long term diet and exercise. That is important context because it shows a best case outcome that the show enabled for some participants.
The data the show produced and what it showed
One of the most striking points Dr. Huizenga made in our conversation is that the show performed more longitudinal metabolic study on reality TV contestants than had ever been done before on a program like that. They tracked contestants for six years and tried to understand why some people were able to keep weight off while others cycled back.
The headline findings were simple but revealing. On average, roughly half of the people studied regained most of the weight they had lost. The other half maintained substantial weight loss. When the team dug into the differences between those who maintained and those who did not, one of the clearest distinctions was daily activity time. The group that maintained their weight was exercising roughly 70 to 75 minutes a day on average. The group that regained most of their weight was exercising on the order of 15 to 20 minutes a day on average.
That is not a moral judgment. It is a measurable behavioral correlate. Time spent moving appears to be a strong predictor in those cohorts for maintaining large weight losses. It also helps explain why sudden, extreme reductions in calorie intake without sustained lifestyle supports are so often followed by regain.
Did the show break people’s metabolisms? The NIH study controversy
This is the part of the story that caused a lot of pain, confusion and bad press. A widely circulated study suggested that contestants came off the show with permanently damaged metabolisms. The claim spread widely, amplified in media outlets, and had real human consequences. Participants called Dr. H in tears, convinced that they had been permanently broken.
Dr. Huizenga told me that, after reviewing the methods and comparing to replicative work done by other investigators, it appears that the key finding of permanent metabolic damage was an artifact of a measurement error. The critical error happened at the first metabolic rate measurement, which was made on the contestants the day they arrived at the ranch. They had traveled, they were nervous, they had not slept well, they were amped up and excited. Those circumstances virtually guaranteed that their resting metabolic rate would be higher than their normal baseline.
What followed was a compare and contrast in which subsequent metabolic rates, conducted under calmer conditions, looked lower in comparison. When other groups attempted to replicate the finding, they could not. When the initial high reading is discounted as an anomalous measurement, the long term picture changes substantially. The conclusion now, as Dr. H explained to me on air, is that the original assertion of permanent metabolic damage appears to be incorrect.
Two points are crucial here. First, there is still a legitimate physiological phenomenon called metabolic adaptation, or adaptive thermogenesis, that occurs when people lose weight. Their bodies need fewer calories to maintain a smaller mass, and some people experience a drop in energy expenditure beyond what would be predicted by weight loss alone. This makes maintained weight loss harder for many people. Second, the idea that a TV intervention permanently wrecked someone’s metabolism was not supported once the measurement error was acknowledged and replication failed to reproduce the original dramatic claim.
I want to be very clear: metabolic adaptation is real. Rapid weight loss, especially when accompanied by a loss of lean muscle mass, often reduces the number of calories a person burns at rest. That is one reason gradual, sustainable approaches that prioritize strength training and protein intake make biological sense. But permanent destruction of metabolic function is not what the corrected data show.
What went wrong with public perception
There are a few reasons the myth spread. Media outlets, including very reputable sources, did not fully interrogate the methodology. The early paper used results that looked damning, and those results made a compelling headline. The human element made it worse. Contestants were understandably emotional. The combination of a bad methodological read, rapid amplification, and real patient distress created a feedback loop.
Dr. H told me he felt a deep regret that he had not been able to intervene more aggressively in the public conversation to clarify the science sooner. He also made the point that we should be cautious in how we present longitudinal metabolic data from small, intensively studied cohorts, because the public may generalize findings in ways that cause needless fear.
Aftercare, responsibility and the reality of television
Another major theme we tackled is aftercare. Danny and other contestants raised the point in the docu-series that people were sent home after intense weight loss with insufficient long term clinical or psychological support. That raises ethical questions. If a production benefits commercially from transforming someone’s body and life, is there a moral obligation to underwrite multi year follow up that supports long term maintenance?
Dr. Huizenga stressed that he personally did not profit from the show beyond his hourly pay. He attempted to follow contestants and charted their progress for the first six years. He phoned many of them. He regrets that the program could not provide more structured aftercare. Those regrets are important because they point toward solutions.
It is one thing to design an intense, controlled, medically supervised environment for short term results. It is another thing to translate that environment into long term habits in a real, messy life. Aftercare needs to be real, affordable and multidisciplinary. It should include behavioral health, access to trained exercise professionals, periodic medical follow up, and financial supports where necessary. Without that, we risk setting people up for relapse and the psychological consequences that follow.
What the science recommends for preserving metabolic health during large weight loss
Based on the combination of the show’s data and the wider literature in obesity medicine, here are the practical messages I emphasized during the interview and want to expand on here.
- Prioritize strength preservation – When people lose weight rapidly, a significant fraction of that weight loss can be lean body mass. Preserving muscle via resistance training and adequate protein intake helps sustain resting energy expenditure.
- Aim for sustained activity – The Biggest Loser follow up suggested maintainers averaged 70 to 75 minutes of exercise per day. That does not mean everyone must do that exact amount, but it shows the scale of daily movement that supports long term weight maintenance after large losses. Building up to substantial daily movement matters.
- Use a moderate calorie deficit – Extreme caloric restriction elevates the risk of muscle loss, hormonal changes, and plateaus. A moderate deficit paired with exercise reduces those risks while being more sustainable.
- Make mental health part of care – Therapy, group support, and ongoing coaching reduce relapse risk and help people navigate identity shifts after big body changes.
Specific exercise recommendations
If you are trying to lose a lot of weight and preserve metabolic function, I recommend this balanced, progressive program. This is the plan I discussed with several clinicians and adapted from evidence based approaches. Adjust intensity for your fitness and medical history and get clearance from your clinician.
- Daily movement baseline – Start aiming for 60 minutes of structured activity per day and gradually increase to 75 minutes per day if you are aiming for very large sustained losses. That total can include a combination of walking, cycling, structured cardio, and resistance training.
- Resistance training – 3 sessions per week, 45 to 60 minutes each. Focus on compound movements: squats, deadlifts or hinge variations, presses, rows, and lunges. Use 3 sets of 6 to 12 reps for major muscle groups. Progressive overload is important. If you are new to lifting, work with a trainer for 4 to 8 weeks to learn form.
- Aerobic training – 150 to 300 minutes per week of moderate aerobic activity is a reasonable starting point. For people trying to maintain very large losses, accumulating 70 to 75 minutes of moderate to vigorous activity daily may be necessary.
- High intensity interval training – Use sparingly and build up slowly. HIIT can preserve metabolic rate and improve fitness, but it is taxing and should be integrated after a solid base of aerobic fitness is established.
- Low intensity daily movement – Stand, walk, take short activity breaks, and keep daily step counts up. Non exercise activity thermogenesis counts.
Nutrition and protein targets
Nutrition will always be individualized, but there are principles that help preserve metabolic rate and lean mass. Here is the structure I discuss with clinicians and individual patients.
- Protein – Consume sufficient protein to preserve muscle. Aiming for 1.2 to 1.6 grams per kilogram of body weight per day is reasonable for most people undergoing weight loss, and in some cases up to 1.8 grams per kilogram may be appropriate if resistance training intensity is high. For example, a 90 kilogram person could target 108 to 144 grams of protein per day.
- Quality of calories – Prioritize whole foods, vegetables, legumes, lean proteins, whole grains and healthy fats. Minimize ultra processed, hyperpalatable foods that drive overeating.
- Calorie deficit – Aim for a deficit that produces steady weight loss, typically 500 to 1000 calories per day under many clinical algorithms, but personalize this based on baseline energy expenditure and medical comorbidities. Larger deficits can be used short term under medical supervision, but only with muscle sparing strategies in place. Larger deficits, or approaches like intermittent fasting, can be used short term under medical supervision, but only with muscle sparing strategies in place.
- Fiber and hydration – Increase fiber intake to support satiety and microbiome health. Drink adequate water, which assists with performance and some appetite regulation.
Vitamins, supplements and exact dosages I discuss with clinicians
I know this is the section people read first. Supplements do not replace diet and exercise but they can support recovery, bone health, immune function and energy, especially after significant weight loss. I will be precise. These are dosages I typically discuss with clinicians and patients, drawn from common clinical practice and safety ranges. Always discuss with your clinician before starting a new supplement, especially if you are pregnant, breastfeeding, have kidney disease, take medications, or have other medical conditions.
- Daily multivitamin – Take one standard adult multivitamin daily. Choose one that provides 100 percent of most B vitamins, vitamin C and vitamin E in amounts consistent with RDAs. A multivitamin helps prevent deficiencies during caloric restriction.
- Vitamin D3 – 2,000 international units per day is a reasonable maintenance dose for many adults. If you are deficient, clinicians often prescribe 5,000 IU per day temporarily or 50,000 IU weekly for a limited time until repletion is confirmed by a blood test. Check 25 hydroxyvitamin D levels and tailor dosing to reach a target of 30 to 50 ng per milliliter depending on clinical guidelines.
- Omega-3 fish oil (EPA+DHA) – 1,000 to 2,000 milligrams per day of combined EPA and DHA. This dose supports cardiovascular health and may reduce inflammation. Choose a molecularly distilled product that is third party tested for purity.
- Calcium – Aim for total calcium intake of 1,000 to 1,200 milligrams per day from diet and supplements combined. If you need supplemental calcium, take no more than 500 milligrams in a single dose and spread doses through the day for better absorption. Do not exceed total intakes recommended by your clinician.
- Magnesium – 200 to 400 milligrams per day of magnesium citrate or magnesium glycinate at bedtime can help muscle recovery and sleep. Magnesium oxide is less bioavailable. One option I often recommend is CanPrev’s Magnesium, which is well absorbed and formulated for daily use. Magnesium oxide is less bioavailable.
- Vitamin B12 – If you are deficient or at risk due to age or certain diets, 500 to 1,000 micrograms of methylcobalamin daily is a common supplemental dose. Some clinicians give 1,000 micrograms weekly via injection depending on deficiency severity.
- Protein supplement – If dietary protein targets are hard to meet, use a whey protein isolate or a vegan protein powder to add 20 to 40 grams of protein per serving. Typical usage is one to two shakes per day depending on needs.
- Creatine monohydrate – 3 to 5 grams per day is an evidence backed dose to support muscle strength, especially during caloric restriction. Creatine is safe for most people with normal kidney function and is among the best studied supplements for preserving lean mass.
- Probiotic – A multi strain probiotic with 10 to 50 billion CFUs per day can support gut health. Probiotics may modestly affect weight regulation indirectly via inflammation and gut barrier function. Choose clinically tested strains when possible.
Timing notes
- Take vitamin D3 and omega-3 with a meal containing fat for better absorption.
- Split calcium doses to 500 milligram increments if using >500 milligrams supplemental calcium per day.
- Take magnesium in the evening if it helps you relax and sleep.
- Use creatine consistently every day; a loading phase of 20 grams per day split across four doses for 5 to 7 days is optional but not required. The maintenance dose is 3 to 5 grams per day.
Safety first
Please note these doses are intended as general guidance. They are within common clinical ranges but individual needs vary. Patients with kidney disease, hypercalcemia, or other disorders need specialized dosing. Pregnancy and breastfeeding require careful review. Check medication interactions, such as omega-3 and anticoagulants, and monitor labs when appropriate, including vitamin D levels and renal function.
How to measure your metabolic rate accurately
If you want an accurate resting metabolic rate assessment, here is what I recommend based on standard practice and the problems the Biggest Loser data exposed.
- Do not measure on a day when you have just traveled a long distance or are highly stressed. Arrive rested and with normal sleep the prior night.
- Fast overnight for at least eight hours before the test. Avoid caffeine, nicotine and vigorous exercise for 24 hours prior to testing.
- Rest quietly for 20 to 30 minutes before the measurement in a thermoneutral environment.
- Use indirect calorimetry in a clinic or research setting when possible. This uses gas exchange to estimate resting energy expenditure and is the gold standard for clinical measurement.
- If you cannot get indirect calorimetry, use validated equations such as the Mifflin St Jeor equation, and apply corrections for activity and body composition. Remember these are estimates not absolute truths.
- If you are participating in research or an intervention, keep your baseline collection conditions consistent with follow up collections to avoid the same error that misled some of the early reporting on The Biggest Loser.
Practical, step by step maintenance plan after rapid weight loss
One reason contestants struggled after the show is that there was not always a clear, affordable and scalable maintenance plan. Here is a pragmatic 12 month plan I believe clinicians and patients can implement to prevent the yo yo effect and protect metabolic health.
- Month 0 to 1: Stabilize
- Transition from rapid weight loss to stabilization with a modest increase in calories to maintenance levels as determined by a clinician or after indirect calorimetry.
- Start a protein target of 1.2 to 1.6 grams per kilogram per day.
- Begin resistance training 2 to 3 times per week with a qualified trainer or under clinician supervision.
- Begin prescribed supplements after review with a clinician.
- Months 2 to 6: Build habits
- Increase daily movement toward 60 minutes per day total, including structured aerobic activity 3 to 5 times per week.
- Use a weekly check in system with a coach or clinician. This can be telehealth.
- Implement behavioral therapy sessions every 2 weeks for the first 3 months, then monthly.
- Monitor weight trend weekly, not daily. Use a moving average to reduce the emotional volatility associated with daily fluctuations.
- Months 6 to 12: Support and scale
- Scale up daily activity toward 70 to 75 minutes per day if you have large losses to maintain. Spread this across resistance and aerobic training.
- Transition to monthly clinician follow up and maintain therapy or peer group meetings monthly or bi monthly.
- Reassess labs at 6 months and adjust supplements accordingly, especially vitamin D and B12.
- Consider a maintenance meal plan that allows flexibility. Rigid diets increase relapse risk. For long-term structure and accountability, programs like our Integrate protocol can help bridge the gap between initial transformation and sustainable maintenance.
What role should television producers and clinicians play

There is an ethical dimension here. Shows create a controlled environment that produces impressive short term results. If they are using medical staff and participants as part of their narrative, there is an argument that producers have some continuing responsibility to ensure participants get long term support. That support can take multiple forms: funded therapy, connections to community resources, extended nutritional counseling, and periodic medical monitoring. It does not have to be indefinite but should be meaningful and tailored.
Dr. Huizenga told me he tried to call contestants and charted them for the first six years. That kind of follow up is rare in media. The show’s structure allowed for extensive study which in turn produced data that both informed practice and created controversy. Going forward, producers should build aftercare into the budget and design of transformation shows.
How to talk to your clinician about large losses and maintenance
When you meet with your clinician after a substantial weight loss intervention, bring these specific items to the conversation. They will help your clinician design an appropriate plan and reduce the risk of being dismissed or poorly supported.
- Ask for a resting metabolic rate assessment and clarify the testing conditions.
- Request baseline labs: thyroid function, fasting glucose or hemoglobin A1c, basic metabolic panel, liver function tests, vitamin D 25 hydroxy level, B12 level, and lipid panel.
- Discuss protein targets and ask for a referral to an evidence based registered dietitian if needed.
- Request a structured resistance training referral and an exercise prescription.
- Ask for a mental health referral and a plan for regular follow up, including behavioral strategies for emotional eating or body image concerns.
- Discuss the use of supplements and the exact dosing, and ask for lab monitoring plans if supplement doses are above the typical RDA range.
Realistic expectations and personal stories
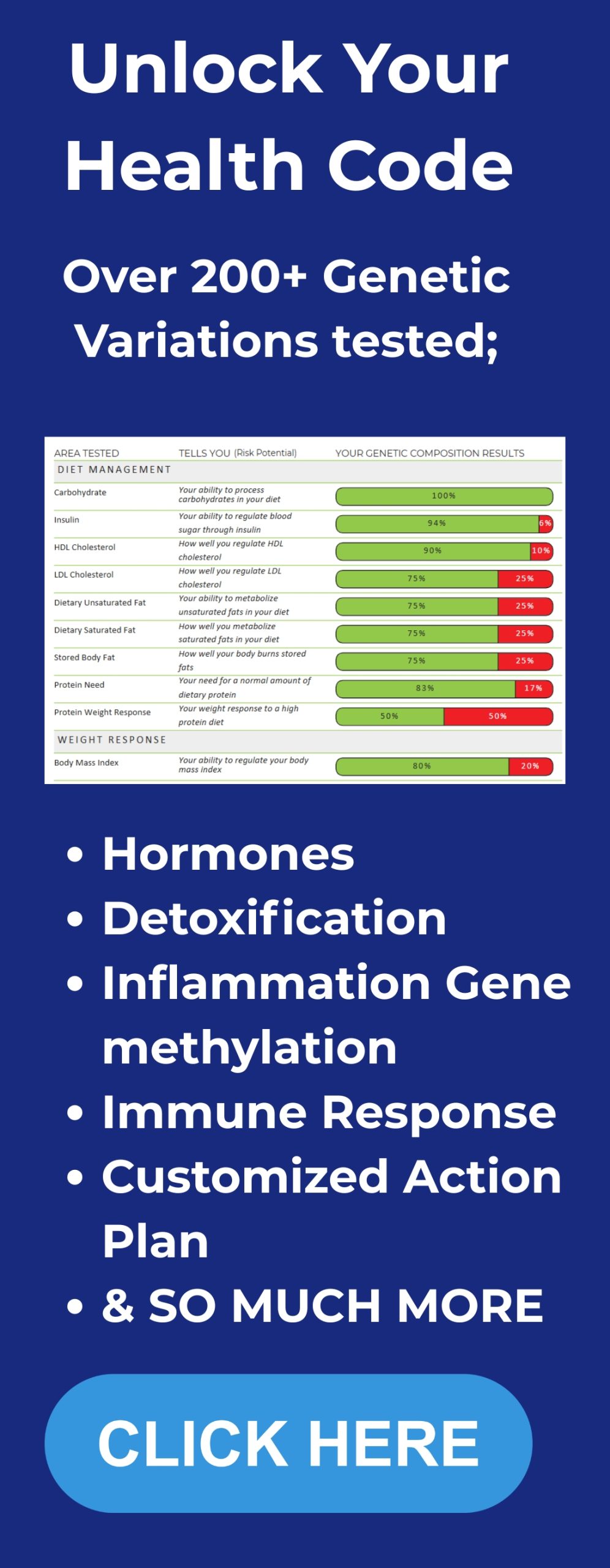
The human element of the docu-series and our interview echoed a broader truth: people respond differently to interventions. Some of that is genetics—which is why getting personalized DNA insights can help tailor nutrition and exercise plans—some is life circumstances, some is the combination of favors and misfortunes each person experiences.
My job in the interview, and in this article, is to bring clarity. Rapid transformations are possible. They can be medically supervised to reduce immediate risk. But long term success depends on building lifestyle patterns that can be sustained in the unpredictability of everyday life. That includes realistic exercise targets, dietary patterns that meet nutritional needs, psychological support, and a plan for ongoing medical monitoring.
Policy implications and the path forward
There are policy lessons embedded in the conversation. Producers should consider mandatory aftercare for contestants who undergo medicalized transformations. Medical societies could issue guidelines for how media partnered interventions should be monitored and what obligations producers and clinicians have after production ends.
In research, we need better replication and more careful public communication. The Biggest Loser story shows how a single methodological misstep can cascade into a cultural narrative that harms participants. Scientists, journalists, and clinicians must work together to ensure public facing claims are accurate and contextualized.
Summary and takeaways
Let me summarize the most important practical points I want you to remember from this long discussion.
- Metabolic adaptation is real, but permanent metabolic destruction from The Biggest Loser style interventions is not supported by corrected data.
- Measurement matters. The original claim of permanent damage was likely driven by an anomalous baseline measurement on the day contestants arrived. Ensure consistent conditions for metabolic testing.
- Daily activity matters a lot. People who maintained large losses averaged roughly 70 to 75 minutes of exercise per day. That level of movement is a strong correlate of maintenance among those cohorts.
- Preserve muscle. Resistance training and sufficient protein are essential to protect resting energy expenditure during weight loss.
- Aftercare is an ethical requirement. If programs produce dramatic transformations, they should provide sustained support, including mental health services, exercise coaching, and medical monitoring.
- Supplements can help, but they are adjuncts. I provided specific dose ranges for commonly used supplements. Use them under clinical supervision.
FAQ
Q 1: Can extreme weight loss permanently damage your metabolism?
A: No, permanent destruction of metabolic function is not supported by corrected data from the Biggest Loser studies. Metabolic adaptation is a normal biological response to weight loss, involving decreases in resting energy expenditure and other hormonal changes that make maintenance harder. Those adaptations are often reversible or manageable with strategies that preserve muscle, ensure adequate nutrition, and incorporate sustained activity and behavioral support.
Q 2: How much exercise do I need to maintain big weight losses?
A: The follow up research from contestants suggests maintainers averaged 70 to 75 minutes of exercise per day. That is a substantial amount of activity but it can be accumulated through a mix of resistance training, aerobic exercise, and daily movement. Not everyone needs that exact amount, but significant daily movement is strongly correlated with long term maintenance after large losses.
Q 3: Which supplements should I take and what are the exact dosages?
A: Here are the supplements and dosages I discussed. These are common clinical recommendations but discuss with your clinician before starting them.
- Multivitamin: one daily standard adult multivitamin
- Vitamin D3: 2,000 IU per day typical maintenance; higher doses for deficiency under supervision
- Omega 3 EPA+DHA: 1,000 to 2,000 milligrams per day combined
- Calcium: total intake 1,000 to 1,200 milligrams per day from diet and supplements combined
- Magnesium: 200 to 400 milligrams per day, preferably magnesium glycinate or citrate
- Vitamin B12: 500 to 1,000 micrograms per day if deficient or at risk; injections in certain cases
- Protein supplement: 20 to 40 grams per serving to reach a target of 1.2 to 1.6 grams per kilogram per day
- Creatine monohydrate: 3 to 5 grams per day for muscle strength and retention
- Probiotic: 10 to 50 billion CFU per day with multi strains
Q 4: How should I measure my metabolic rate accurately?
A: Use indirect calorimetry in a clinic under standardized conditions: overnight fast, avoidance of caffeine and exercise, rested and thermoneutral environment. If you cannot get that, use validated equations and ensure consistent testing conditions across time points to reduce measurement artifacts.
Q 5: If I want to lose a lot of weight, what is the safest approach?
A: Work with clinicians and multidisciplinary teams. Prioritize a moderate caloric deficit, strong protein targets, resistance training, aerobic training, and behavioral therapy. If considering rapid or medically supervised programs, ensure there is an aftercare plan that includes medical follow up and psychological support.
Q 6: What should producers of transformation shows do differently?
A: Producers should build aftercare into program budgets, provide funded therapy, provide access to nutritionists and exercise professionals after filming, and commit to multi year follow up where possible. Clinicians working on these shows should insist on responsible public communication of research findings and consistent measurement protocols.
Q 7: Where can I find more resources?
A: I recommend starting with evidence based obesity medicine resources, reputable nutrition societies, and certified exercise professionals. If you watched our NewsNation segment, the accompanying docu-series Fit for TV provides context, and Dr. Huizenga and former contestants offer rich first person perspectives.
Final thoughts
I have sat with clinicians, contestants and researchers who were directly involved with The Biggest Loser era and the subsequent debate. What I heard repeatedly is that people got better and worse at different times, that the science evolved, and that some of the media messaging was harmful. My job in public conversations is not to pick sides but to clarify what we know, what we do not know, and what actionable steps help people live healthier lives.