Today we’re diving into a topic that’s become more and more common in health discussions: cannabis. While often talked about in the context of relaxation or recreation, the reality is much more complex and much more relevant for anyone who cares about long-term health and performance. From the way cannabis interacts with your brain and body, to the differences between strains and compounds, to the potential risks and strategies to reduce harm, the science paints a nuanced picture. In this post, we’ll break down what the latest research reveals and who might be at higher risk. We’ll also explore practical, evidence-based protocols covering vitamins, supplements, and lifestyle strategies with specific dosages that can support your wellbeing. Let’s dig into the science and see what’s really going on beneath the surface.
Table of Contents
- How I think about cannabis: an overview
- Strains and types: sativa, indica, hybrid, and the Type 1/2/3 system
- Why cannabis affects us: the endocannabinoid system
- Pharmacokinetics and persistence
- What cannabis does to your brain and body – the predictable effects
- Creativity, dopamine, and cannabis
- How cannabis alters speech and motor patterns
- Cannabis, sex, hormones, and fertility
- Smoking and vaping: vascular and pulmonary harm
- Why I am emphatic about avoidance
- Adolescence, cortical thinning, and risk of psychosis
- The paradox of tolerance and worsening anxiety over time
- Putting it into practice – my Better Life approach
- FAQ
- Final thoughts
How I think about cannabis: an overview
Cannabis is not a single drug. It is a plant family that contains hundreds of biologically active compounds. The two most widely discussed are THC (Delta-9-tetrahydrocannabinol) and CBD (cannabidiol). THC is the primary psychoactive compound, the one largely responsible for the subjective “high.” CBD does not commonly produce a strong high but has biologic actions that interact with the same systems in our bodies. There are also other cannabinoids such as CBN and dozens of minor cannabinoids that remain under study. The plant also includes hundreds of non-cannabinoid compounds that can alter aroma, experience, or even physiology.
When I help people think about cannabis, I break the discussion down to a few practical variables:
- Which strain or variety – sativa, indica, or hybrid
- THC to CBD ratio – commonly classified today as Type 1 (THC-dominant), Type 2 (mixed ratio), Type 3 (CBD-dominant)
- Method of delivery – smoked, vaped, edible, tincture, transdermal
- Dosage and frequency of use – single/occasional use versus chronic use (generally twice a week or more)
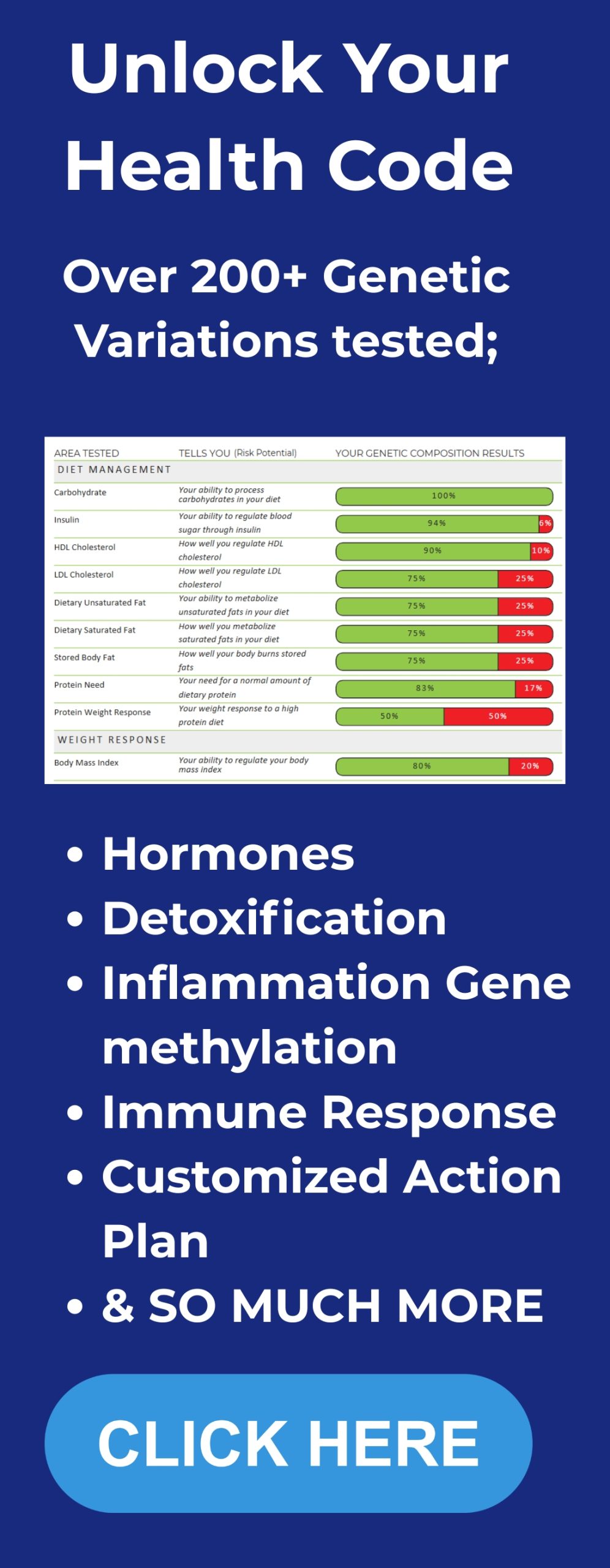
- Age, sex, genetics, and mental health vulnerability — genetics in particular can influence how cannabis affects you. If you want to dig deeper, you can get personalized DNA insights to better understand your risks.
Strains and types: sativa, indica, hybrid, and the Type 1/2/3 system

Sativa and indica started as botanical descriptions. Sativa plants tend to be taller with longer leaves and are historically associated with head-biased effects – stimulation, alertness, talkativeness, and sometimes a narrowed focus. Indica plants are shorter and denser, and their effects are more body-biased – relaxation, sedation, and sleep facilitation.
Modern growers hybridize strains liberally. Because the chemical composition is what drives human experience, many clinicians now think in terms of Type 1, Type 2, and Type 3:
- Type 1: THC-dominant (higher psychoactive potency)
- Type 2: Mixed THC-CBD ratios
- Type 3: CBD-dominant (minimal intoxicating effect for most people)
Understanding the ratio of THC to CBD is critical to predicting likely effects, although individual responses can differ widely. A pure sativa Type 1 is likely to feel energizing to many people but can provoke anxiety and paranoia in some. A pure indica Type 1 can feel deeply sedating and can impair short-term memory and planning.
Why cannabis affects us: the endocannabinoid system
The real reason cannabis has effects is that humans (and other animals) have an endocannabinoid signaling system built into our biology. We produce internal cannabinoids such as anandamide and 2-AG. These endogenous cannabinoids bind to receptors called CB1 and CB2 that are present throughout the brain and body. THC and CBD bind to these same receptors, but often with much greater potency and duration than the internal compounds.
Key points I want you to remember about this system:
- CB1 receptors are highly enriched in the nervous system, especially the brain. They influence mood, cognition, appetite, memory, motor control, and more.
- CB2 receptors are more common in peripheral tissues and immune cells. They influence inflammatory and immune responses, among other things.
- Endogenous cannabinoids modulate synaptic transmission retrogradely – they are released from postsynaptic cells to act back on presynaptic terminals and regulate neurotransmitter release. This fine-tuning is essential for normal brain development and function.
- When you introduce THC or high-potency cannabinoids repeatedly, these potent exogenous molecules outcompete endogenous cannabinoids and can blunt or dysregulate the system over time.
Pharmacokinetics and persistence
Cannabis compounds are lipophilic. They enter the bloodstream rapidly when inhaled – within seconds to a minute they reach the brain. Peak psychological effects typically occur at 30 to 60 minutes after inhalation. The acute effects usually last 3-4 hours but metabolites can remain detectable in fatty tissue for weeks. In practice, THC and related metabolites can be detected for up to 80 days in individuals with significant body fat or frequent use.
What cannabis does to your brain and body - the predictable effects

Some effects are quite consistent across users and delivery systems, while others are highly variable. When I coach people I separate predictable physiologic effects from subjective variations.
Predictable physiologic effects
- Memory impairment – especially short-term memory linked to hippocampal suppression
- Motor and coordination slowing – suppression of basal ganglia and cerebellar circuits
- Red eyes and dry mouth – reduced tear and saliva secretion
- Munchies – stimulation of hypothalamic circuits and appetite networks
Variable subjective effects
Sativa-type use commonly produces head-centered effects: alertness, talkativeness, narrowed focus, and subjective creativity. Indica tends to be body-centered: sedation, relaxation, and sleep facilitation. Both sativa and indica can either lower anxiety or provoke anxiety and paranoia. Which outcome you experience depends on dosage, THC to CBD ratio, your genetics, prior exposure, and pre-existing mental health conditions.
Creativity, dopamine, and cannabis
Creativity is not a unitary process. When researchers study creativity they commonly distinguish divergent thinking – a brainstorming, idea-generating mode – and convergent thinking – the synthesis and selection process that makes ideas actionable. Dopamine is a key modulator here. Moderately elevated dopamine promotes divergent thinking. Low dopamine promotes convergent reasoning. Too much dopamine is again detrimental to divergent thinking. Cannabis can elevate dopamine in certain mesocorticolimbic circuits and therefore may increase the probability of divergent thinking for some people. But the literature shows mixed results.
A key study titled “Inspired by Mary Jane?” found that cannabis users showed greater creativity on testing when they were not acutely intoxicated. The authors concluded that the link between cannabis and creativity is largely driven by personality differences such as openness to experience rather than a direct boosting effect on neural creativity circuits. In my practice this means:
- If you respond to cannabis with reduced anxiety and increased openness, it can facilitate brainstorming and creative exploration.
- If cannabis causes anxious rumination or paranoia for you, it will interfere with creativity.
How cannabis alters speech and motor patterns
Speech is movement. The basal ganglia and cerebellum coordinate fine motor execution, including the muscles of articulation. Chronic cannabis use (operationally defined in many studies as twice weekly or more) is associated with measurable differences in speech production: reduced spectral tilt indicating lower vocal effort, changes in timing and enunciation, and a tendency toward drawn-out syllables. Some of these changes are evident even when chronic users are not acutely intoxicated.
Cannabis, sex, hormones, and fertility
Sexual desire and function are regulated by a balance of dopamine, prolactin, testosterone, oxytocin, and other hormones and circuits. Cannabis has divergent effects here, and the data can be confusing unless you look closely at the details.
One fMRI study found that the key variable was prolactin reactivity. Participants whose prolactin rose after acute cannabis intoxication showed diminished nucleus accumbens activation and reduced sexual arousal. Those whose prolactin did not rise experienced increased activation and arousal. In other words, cannabis increases sexual arousal for some people and reduces it for others depending on their hormonal response.
Longer term, smoking cannabis more than twice weekly is consistently associated with increased prolactin, reductions in luteinizing hormone and follicle stimulating hormone, and reduced testosterone in many studies. Chronic use has been linked to lowered sperm motility and function in men and altered ovarian function in women in several reports. These are important considerations if you are trying to optimize fertility.
Smoking and vaping: vascular and pulmonary harm
Separately from cannabinoid-specific effects are harms of inhaling smoke or aerosols into the lungs. Smoking or vaping tobacco or cannabis impairs endothelial cells that line blood vessels and capillaries. That impairment reduces cerebral blood flow over time, increases stroke risk, reduces lung function, harms peripheral circulation, and contributes to sexual dysfunction via poorer genital blood flow.
If you are looking to minimize harm and you are not pregnant or adolescent, ingestion via controlled edible formulations provides a consistent dose and avoids inhalation injury, but edibles have their own pharmacokinetic realities: delayed onset, unpredictable metabolism, and prolonged duration.
Why I am emphatic about avoidance

CB1 receptors are expressed throughout brain development. Endogenous cannabinoids are abundant in the fetus and are essential regulators of neural proliferation, axonal outgrowth, synapse formation, and wiring. Repeated activation of CB1 by exogenous cannabinoids during gestation or early childhood risks interfering with fundamental neurodevelopmental events.
The latest surveillance data indicate that around 15 percent of pregnant people in some surveys report cannabis use during pregnancy. From my perspective and the view expressed by many obstetricians and pediatricians, that is a serious public health concern. Because cannabis compounds are lipophilic and cross the placenta and pass into breast milk, I recommend avoidance of cannabis of any form during pregnancy and lactation unless under tightly controlled clinical care and with direct guidance from your medical team.
Adolescence, cortical thinning, and risk of psychosis
The developing brain continues to undergo major maturation processes well into the mid-twenties. CB1 receptor occupancy during adolescence, especially when repeated with higher potency THC products, has been linked to accelerated cortical thinning in prefrontal areas that subserve planning, emotional regulation, and executive control. Large consortium data show a dose-response relationship: the more frequent the adolescent use, the greater the change in cortical thickness.
Heavy cannabis use in adolescence is associated with elevated risk of later psychosis, particularly in individuals with genetic vulnerability. Systematic reviews show that early onset and high potency use increase risk substantially. My practice and Betterlifeprotocols.com protocols emphasize prevention here: no recreational cannabis for anyone under 25, and careful harm reduction counseling for young adults.
The paradox of tolerance and worsening anxiety over time
Repeated CB1 activation by potent exogenous cannabinoids leads to receptor desensitization and downstream signal attenuation. This manifests clinically as tolerance – progressively more drug required to achieve the same perceived benefit. Over months this pattern is associated with worsening baseline anxiety and depressive symptoms in a subset of users. Paradoxically, a drug used to reduce anxiety can become a driver of chronic anxiety and depression if used frequently and in high doses.
Putting it into practice - my Better Life approach
If you want a pragmatic path forward I divide recommendations into three categories:
- Immediate safety rules
- Evidence-based supplementation stack to support recovery or mitigation
- Behavioral and medical strategies to reduce harm and restore brain health
Immediate safety rules
- If you are pregnant or breastfeeding avoid cannabis in all forms.
- If you are under 25, avoid recreational cannabis use. The developing brain remains vulnerable.
- If you have a strong family history of psychotic disorders like schizophrenia or bipolar disorder, avoid cannabis, especially high THC products.
- Avoid smoking or vaping cannabis because of endothelial and pulmonary harm. If you are going to use, choose verified, laboratory-tested edible or measured tinctures and start at the lowest dose.
My core supplement stack for people reducing or quitting cannabis
The supplements below are the protocol I discuss at Betterlifeprotocols.com as a starting point for supporting recovery of sleep, mood, cognition, and metabolic health. These are general recommendations and not individualized medical advice. Please review with your clinician before starting supplements, especially if you take prescription medications.
Daily foundational stack
- AG1 or a comprehensive multinutrient formula: once daily in the morning mixed with water. AG1 delivers a multivitamin, minerals, adaptogens, and a probiotic base that supports baseline nutrition. I use one scoop per day as directed on the product label.
- Vitamin D3 with K2: 2,000 to 5,000 IU vitamin D3 daily with 100 mcg vitamin K2 (MK-7). If you’re unsure why maintaining optimal levels matters so much, see our guide on why you need more vitamin D. I generally recommend 5,000 IU per day if you have low sun exposure and are not monitored, and a minimum 2,000 IU/day for maintenance. If you have recent labs, titrate to achieve 25-hydroxyvitamin D in the range 40-60 ng/mL per InsideTracker or your provider. Take with a fat-containing meal.
- Omega-3 fish oil (EPA/DHA): combined EPA + DHA of 1,000 to 2,000 mg per day. I most commonly use 1,000 mg for maintenance and 2,000 mg during periods of mood dysregulation or heightened inflammation. Take with meals.
- Magnesium glycinate: 200 to 400 mg at bedtime to improve sleep onset and sleep quality. I often recommend CanPrev’s Magnesium as a reliable option. You can also learn more about why not all magnesium is the same. Magnesium supports neuronal homeostasis and can blunt overactivity. Start at 200 mg and increase to 400 mg if tolerated.
- B-complex or methylated B12: 1,000 mcg sublingual methylcobalamin every morning on days when mental fatigue or low motivation is present. A daily B-complex can be used at label doses if you have no contraindications.
- Zinc: 15 to 25 mg per day with food, not at the same time as magnesium. Zinc supports hormonal balance and immune function. Avoid prolonged high doses above 40 mg/day without monitoring.
- Probiotic: use the probiotic in AG1 or a separate multi-strain probiotic delivering at least 10 billion CFU daily. Gut health supports inflammation control and brain communication.
- Vitamin C: 500 mg once daily as a general antioxidant support.
Targeted support for cessation, cravings, or mood support
- N-acetylcysteine (NAC): 600 mg twice daily (morning and evening) for 30 to 90 days in individuals struggling with cravings or compulsive patterns. NAC supports glutathione synthesis and has preliminary evidence as a harm reduction aid for several substance uses. Discuss with your provider if you have asthma or take nitroglycerin or other special medications.
- L-theanine: 100 to 200 mg in the afternoon or evening to relax without sedation and to blunt anxiety spikes.
- Creatine monohydrate: 3 to 5 grams daily to support brain energy metabolism. This is useful in individuals with chronic depressive symptoms and cognitive sluggishness. Ensure adequate hydration.
- Phosphatidylserine: 100 to 300 mg daily as a cognitive support during withdrawal or when memory is impaired.
I often advise combining these targeted agents for one to three months while emphasizing lifestyle changes and then reassessing. NAC is the one compound I use most often when cravings are the primary problem; magnesium and sleep hygiene are my go-to when insomnia is central.
Lifestyle prescriptions I prioritize
Supplements are useful but they amplify what good lifestyle does. Below is the behavioral protocol I recommend at Betterlifeprotocols.com for individuals stopping or reducing cannabis.
- Sleep first – prioritize a fixed sleep window and use NSDR (non-sleep deep rest) exercises as needed to facilitate falling back asleep. Begin with an NSDR session when you wake in the middle of the night or use the 10-minute NSDR in the morning to restore dopamine related motivation. Practice nightly sleep hygiene: light exposure in the morning, hot shower 60 to 90 minutes before bed for thermoregulation, and avoid bright screens in the hour before bed.
- Cardiovascular exercise – 150 minutes per week of moderate aerobic exercise or 75 minutes high-intensity; ideally spread across 4 to 6 sessions. Exercise supports endothelial health, neurogenesis, and mood stabilization. It helps to clear inflammatory markers and supports blood flow to prefrontal cortex.
- Resistance training – two to three times weekly to support hormonal health, metabolic function, and cognition.
- Nutrition – emphasize whole foods, adequate protein, colorful vegetables for polyphenols, omega-3 rich fish, and consistent meal timing to stabilize glucose. If you’re working toward long-term changes, consider joining our Integrate program for structured support. Levels continuous glucose monitoring can help optimize meals for metabolic stability.
- Social connection and purposeful work – these protect against depression and reduce the attractiveness of substances as coping tools.
- Mental health support – cognitive behavioral therapy or coaching can reduce reliance on cannabis for mood regulation.
How long will it take to recover after quitting
Recovery is variable. Acute withdrawal, including sleep disruption, increased anxiety, and craving, typically peaks over a few days to two weeks. Sleep often normalizes in one to three weeks with behavioral support. Cognitive recovery, including improvements in attention and memory, is typically observed over a few months. Structural brain changes seen in adolescents may not fully reverse but some functional recovery is plausible with sustained abstinence, cardiovascular exercise, adequate sleep, and nutrition. If you were a heavy, long-term user, expect a longer recovery window and work closely with a clinician.
FAQ
1. Is cannabis safe?
Short answer: it depends. For adults older than 25 with no personal or strong family history of psychosis and who use infrequently and in low doses, some forms of cannabis can be relatively low risk. For adolescents, pregnant or breastfeeding people, and those with genetic risk for psychosis, cannabis can be harmful. Frequency, potency, delivery method, underlying mental health, and age are the major determinants of risk.
2. Does cannabis increase creativity?
Cannabis can increase divergent thinking for some individuals, often by easing anxiety and increasing openness. However, much of the observed association between cannabis and higher creativity is due to personality traits that predispose to both cannabis use and creativity. There is no universal cognitive enhancement.
3. Does cannabis reduce sexual function?
Cannabis may increase sexual desire in some people and reduce it in others. The hormonal response, particularly prolactin reactivity, predicts the outcome. Chronic heavy smoking tends to increase prolactin and reduce testosterone and may harm fertility and function over time.
4. How long does THC stay in my body?
THC is lipophilic and can stay in fat tissues for weeks. In general it can be detected for up to 80 days in heavy users. Detection windows vary by testing method, body composition, and frequency of use.
5. Which vitamins or supplements should I take if I quit cannabis?
My foundational stack includes a quality multinutrient (AG1 or equivalent) once daily, vitamin D3 2,000 to 5,000 IU plus K2 100 mcg, omega-3 fish oil 1,000 to 2,000 mg combined EPA+DHA, magnesium glycenate 200 to 400 mg at night, zinc 15 to 25 mg daily, and a probiotic at least as provided in AG1. Targeted add-ons include NAC 600 mg twice daily for cravings and L-theanine 100 to 200 mg for anxiety. Discuss these with your clinician, particularly if you take medications.
6. I smoke daily and want to stop. What is the best first step?
Start by setting a clear time-limited cessation plan. Inform close contacts and seek behavioral support. Implement the supplement and lifestyle stack above.
Final thoughts
At Betterlife, I emphasize informed decision-making and harm reduction. For young people and pregnant people the recommendation is clear: avoid cannabis. For adults seeking relief or exploration, consider low-dose, infrequent, and – when possible – non-inhaled formulations from certified sources and pair use with strategies to protect sleep, vascular health, and hormonal balance. And remember, this article is educational and not a substitute for a clinician-patient relationship. Always discuss significant changes to your supplement routine or substance use with a healthcare professional.