Today we’re diving into one of the most powerful levers for health and longevity: metabolic optimization. The science here is advancing rapidly, but the practical takeaways are clear and you can take steps right now to improve glucose regulation, reduce inflammation, enhance sleep, and protect long-term organ health. Drawing on cutting-edge research and expert conversations, we’ve translated complex biology into simple, actionable steps. In this guide, you’ll find science-backed strategies, targeted supplement recommendations, and step-by-step behavioral protocols designed to deliver measurable improvements. Whether you’re looking for lab-level precision or just a clear roadmap for your first 90 days, this playbook will help you take control of your biology and upgrade your health from the inside out.
Table of Contents
- Why unique biology matters
- Core principles I use and teach
- Glucose: how to measure it and practical thresholds
- Exercise: how timing and type interact with metabolic subtypes
- Fiber: the one nutrient you must individualize
- Sleep, REM, routines and metabolic health
- Supplements and doses I discuss with clients
- GLP-1 agonists and weight-loss medications – practical considerations
- Organ aging and the concept of ageotypes
- Whole-body MRI and the value of baselines
- Air quality, environmental monitoring and health
- Wearables, HRV, mindset and what to measure daily
- Acupuncture and somatic interventions
- Mental health, immersive interventions and measurable outcomes
- Micro-sampling and single-drop blood metabolomics
- FAQ – answers I give most often
- Closing: a pragmatic invitation
Why unique biology matters
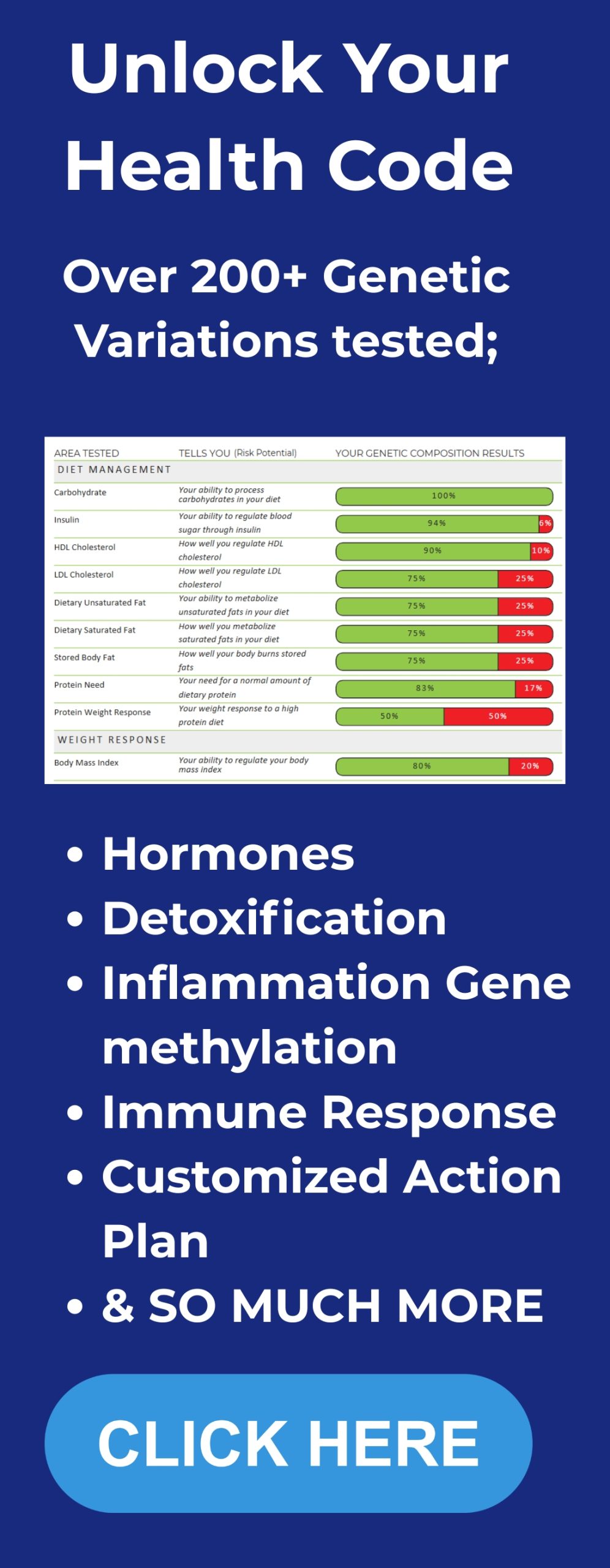
We all come to health choices with different genomes, immune history, microbiomes, sleep habits and behaviors. When a published study, social media post or friend tells you “eat X, avoid Y, take supplement Z” they are giving generalized advice. The central point I want to drive home is this: those generalized rules often work for many people but they can fail for a substantial minority. The right approach is to measure and then act. One way to do that is by getting personalized DNA insights to understand how your genetics shape nutrition, metabolism, and recovery.
Two clear, repeated examples illustrate why measurement matters.
- Glucose responses vary widely. Some people spike when they eat potatoes and not grapes. Some spike to white rice, others do not. Continuous glucose monitoring will show you the unique pattern of your post-prandial glucose excursions. (See a review of CGM utility and outcomes in both diabetic and non-diabetic populations here.)
- Fiber is heterogeneous. Different fibers can produce opposite inflammatory outcomes in different people. Psyllium-type arabinoxylans (for example, metamucil) reduced LDL and APOB in a clinical study, whereas inulin lowered markers for other people. The microbiome and host factors determine the effect. (For example, psyllium fiber has been shown in meta-analyses to reduce LDL cholesterol in controlled trials.)
In short: individualized measurement yields individualized actions. The rest of this article lays out how to measure, what to measure, and specific interventions including exact supplement doses that can be used to move your metrics in a healthier direction.
Core principles I use and teach
- Measure first. Wear a continuous glucose monitor (CGM), use validated wearables for sleep and heart rate variability, and get baseline bloodwork that includes A1C, lipid panel with ApoB, high-sensitivity CRP, and a metabolic panel. If you want to see the bigger picture, here are 10 metabolic trends shaping health and longevity right now.
- Think in ranges and time-in-range. For most people a practical glucose time-in-range target is 70-140 mg/dL and A1c under 5.7% for non-diabetics. For people with diabetes clinical targets differ, and medications are individualized.
- Use lifestyle plus targeted supplementation. Drugs can be powerful, and in many cases life-saving. But drugs are best used together with lifestyle that maintains muscle mass, sleep regularity, and minimizes toxic exposures.
- Segment your metabolism. Diabetes and metabolic dysfunction are not a single condition. There are insulin resistance subtypes at the muscle, liver and fat levels, beta-cell secretory defects, and incretin signaling defects. Knowing your subtype changes what you should do and which drugs will help.
- Iterate fast. Make a change, measure for 7-14 days, and evaluate the effect with your CGM and other metrics. Then tweak again.
Glucose: how to measure it and practical thresholds

My starting point for nearly everyone is a short CGM run. Modern CGMs are available over the counter and record glucose every 5 minutes for 10-14 days. (For context on how CGM technology has evolved and its role in recent clinical use, see this overview.) That density of data is essential to understand your typical glucose range, meal responses and time-in-range.
What I watch closely
- Baseline fasting glucose (typical baseline ~90 mg/dL for many people).
- Post-prandial peaks. For most healthy people peaks under 140 mg/dL within 60 minutes of a meal are acceptable. Sustained peaks above 140 or repeated excursions beyond 180 indicate impaired regulation or diabetes-level excursions.
- Time-in-range percent: how much of the 24-hour day are you between 70 and 140 mg/dL? The more time-in-range the better, and improvements in time-in-range correlate with lower A1c.
- Glucose troughs – very low glucose after a large insulin response can cause fatigue, brain fog and cravings. Aim to avoid large post-peak troughs.
If you are a clinician or have a clinician partner, compare CGM-derived metrics with hemoglobin A1c: <5.7% considered normal; 5.7–6.4% prediabetes; ≥6.5% diagnostic for diabetes in the absence of other causes.
Immediate tactical tools for glucose control
- Brisk post-meal walks. A 15-20 minute brisk walk after a meal blunts post-prandial peaks for most people. If you have limited mobility a series of 1-3 minute exercise snacks or repetitive soleus calf lifts (heel raises while seated) reduces spikes by providing muscular glucose uptake.
- Timing of the large meal. For many people consuming the largest meal earlier in the day is associated with better 24-hour glucose control than loading calories late at night. If you are muscle insulin resistant you can get stronger effects from morning exercise on next-day glucose.
- Macronutrient pairing. Combining high glycemic carbohydrates with intact fiber, protein and healthy fat tends to slow absorption. The magnitude is highly individual – measure and learn what blunts your own spikes.
Exercise: how timing and type interact with metabolic subtypes
Exercise is not one-size-fits-all when it comes to glucose biology. The important distinction is which tissues are causing glucose dysregulation.
- Muscle insulin resistance – If the primary issue is that muscle is not taking up glucose, building and activating muscle matters. Resistance training and periodized morning activity can have outsized benefits.
- Beta-cell secretion defect – If your problem is that your pancreas is not releasing insulin appropriately, adding muscle mass may not directly fix that limitation, because the failure is in insulin release rather than peripheral uptake.
- Hepatic insulin resistance – For liver-centered dysregulation, timing of meals and macronutrient composition can be more powerful.

Practical training routine I use and recommend
- Resistance training 4-6 sessions per week, alternating heavy and light days. Heavy days 3-5 compound lifts at 3-6 reps; light days higher rep metabolic conditioning and mobility.
- Daily low-intensity movement – 15-25 minute post-meal brisk walks to blunt spikes.
- Exercise snacks – for people sitting long stretches: 2-5 minute sets of calf raises, air squats or marching every 60-90 minutes.
Resistance training preserves and grows muscle mass and reduces risk from age-related sarcopenia. It also improves resting metabolic rate and insulin sensitivity over time in many people.
Fiber: the one nutrient you must individualize

Fiber is not a single nutrient. There are multiple fiber chemistries with distinct effects on microbes, bile acid metabolism, cholesterol and the immune system. Clinically useful fiber categories include:
- Psyllium-type arabinoxylans (common supplement: metamucil) – tends to lower LDL cholesterol and ApoB by binding bile acids and altering gut lipid handling. Doses used in trials: 10 – 30 grams per day as a supplement, typically titrated over a few weeks to avoid GI upset.
- Inulin and fructan-type fibers – these are fermentable prebiotics (inulin is common in foods like chicory root, Jerusalem artichoke). Effects can be variable: some people see improved markers, some see increased inflammation depending on their microbiome.
- Beta-glucans (oats, barley, some mushrooms) – often associated with cholesterol-lowering and immune modulation.
- Resistant starch – feeds butyrate-producing microbes; can improve metabolic markers in some people.
Study-based practical approach I use
- Baseline: get a stool microbiome test to learn dominant microbial capabilities if possible.
- Trial single-fiber supplements in a controlled crossover style. Example schedule I use with clients: Week 1-2 baseline; Week 3-5 supplement A at 10 grams daily; Week 6 week washout; Week 7-9 supplement B at 10 grams daily. Increase to 20-30 grams daily slowly only if tolerated.
- Track systemic markers: CRP or hsCRP, LDL, ApoB, CGM time-in-range and subjective GI tolerance. If inflammation markers rise or you feel worse, stop that fiber and try a different one.
Common food sources and supplement examples
- Psyllium husk powder – 5-10 grams once or twice daily (titrate to 10-30 grams per day depending on response). Mix with plenty of water.
- Inulin powder – start with 2-5 grams daily, increase slowly. Many people tolerate 5-10 grams daily; some tolerate 15-20 grams. If bloating and inflammation occur, reduce dose or switch fiber.
- Oat beta-glucan – commonly consumed in food; supplemental beta-glucan dosing 3-6 grams daily used in studies for cholesterol effects.
- Resistant starch – dosing 10-30 grams daily from green banana flour, potato starch, or cooled starchy foods.
Sleep, REM, routines and metabolic health

Sleep timing, consistency and quality are foundational to metabolic control. Key rules I follow and teach:
- Maintain consistent sleep and wake times whenever feasible. Variability in sleep timing correlates with worse glucose control.
- Avoid meals within 2-3 hours of bedtime when possible. Eating immediately before sleep often leaves you with elevated glucose overnight and a worse next-day profile for many people.
- The temperature trick for REM: keep the bed cooler at sleep onset, and warm the bed in the final 1-2 hours of sleep. Clinically observed improvements in REM amount follow this basic thermal pattern for many people.
Over-the-counter sleep supports I use and recommend with typical dosing
- Magnesium threonate – 1,000 to 2,000 mg nightly (commonly marketed products provide elemental magnesium 100-200 mg per dose). I commonly recommend 1,000 mg to start; many products list 1,500-2,000 mg. Use the product label to determine elemental magnesium. Magnesium threonate targets the brain and has supportive evidence for sleep and cognition.
- L-Theanine – 100 to 200 mg before bed to promote relaxation without sedation.
- Glycine – 3 grams taken 30 minutes before bed supports deeper sleep and reduces core temperature.
- Chamomile extract – 200 to 400 mg as a single pre-bed dose for mild sedative effect. Standardized extracts are preferred.
- Saffron extract – 28 to 30 mg daily has clinical evidence for improving sleep and mood in some trials.
- Valerian root – 400 to 900 mg nightly; some people are sensitive. Use only short term and evaluate tolerance.
Important safety notes for sleep supplements
- Start low and go slow. Introduce only one new sleep supplement at a time and assess for morning grogginess or interactions.
- Check for interactions with prescription medications and with alcohol. For example, valerian and sedative medications can interact.
- Watch for digestive side effects with magnesium and glycine. If you have loose stools, reduce magnesium dose or switch formulation.
Supplements and doses I discuss with clients
Below I list the supplements I reference frequently in protocols along with typical doses. These doses reflect the evidence discussed in the scientific literature and the practical experience of clinicians I trust. Always consult a physician before starting new medications or high-dose supplements, particularly if you have kidney disease, liver disease, are pregnant, or are taking multiple prescription medications.
For a curated set of foundational supplements — including magnesium, vitamin D3 with K2, hydrogen tablets, and omega-3s — see our VIP protocol bundle.
Glucose and metabolic support
- Berberine – 500 mg two to three times per day with meals. Berberine mimics some effects of metformin and improves post-prandial glucose. Many people tolerate 500 mg twice daily; clinical trials often use 500 mg two to three times daily.
- Metformin – prescription drug. Typical starting titration is 500 mg daily or twice daily and increased as tolerated up to 1,500 to 2,000 mg daily under physician supervision. Do not self-prescribe. Metformin can cause GI upset; extended-release formulations reduce GI side effects.
- SGLT2 inhibitors – prescription class, e.g., dapagliflozin (Farxiga) used for glucose and cardiorenal benefits. Prescription only. Follow your clinician’s dosing.
- Alpha-lipoic acid – 300 to 600 mg per day for insulin sensitivity and oxidative stress support in some trials.
Cardiometabolic and lipids
- Soluble fiber (psyllium) – 10 to 30 grams per day (start lower, 5-10 grams, and increase). Psyllium reduces LDL and ApoB in controlled trials.
- Omega-3 fish oil – 1,000 to 3,000 mg daily of combined EPA/DHA depending on triglyceride levels. Higher doses are used under prescriber supervision for triglyceride lowering.
- Plant sterols – 2 grams daily can lower LDL modestly; consider if statin therapy not indicated or as adjunct with clinician approval.
Brain, inflammation and longevity-minded supports
- Curcumin – 500 to 1,000 mg per day of a bioavailable formulation for anti-inflammatory support.
- Nicotinamide riboside (NR) or nicotinamide mononucleotide (NMN) – commonly used for NAD+ support with varying doses: NR 250-500 mg daily; NMN 250-500 mg daily. These compounds are active areas of research; long-term benefits in humans are not fully established.
- Metformin – again listed because of clinical and population evidence related to longevity signals. Discuss with your clinician; commonly 500 mg twice daily to start under medical supervision.
I know some of these are prescription-only. I am not suggesting you self-medicate. If you and your clinician decide a drug or supplement is right for you, we use measurement to verify benefit.
GLP-1 agonists and weight-loss medications - practical considerations
Agonists of GLP-1 (e.g., semaglutide, tirzepatide and others) are used for type 2 diabetes and weight loss. They profoundly change appetite signaling and can produce rapid metabolic improvements including A1c decreases and visceral fat reduction. Important points I emphasize:
- These drugs produce super-physiologic GLP-1 receptor activation. Effects include appetite suppression, delayed gastric emptying and weight loss. People report decreased alcohol cravings and some cognitive benefits, though disentangling weight-loss from direct cognitive effects remains an open question.
- Side effects frequently include nausea, especially early in dose escalation. Start low and titrate slowly under clinician supervision. We’ve written more extensively about Ozempic and other GLP-1 drug side effects if you want a detailed breakdown.
- Maintain resistance training while on GLP-1 agonists to preserve muscle mass. People using these drugs can lose lean mass if they do not continue resistance exercise and maintain adequate protein intake.
- Watch for post-meal hypoglycemia if combined with other glucose-lowering drugs like sulfonylureas or if you take metformin/berberine and do not adjust carbohydrate loads.
Organ aging and the concept of ageotypes
Biological age is not monolithic. I prefer the concept of ageotypes – organ or pathway specific aging patterns that show up in blood proteomics and metabolomics. Examples:
- Cardio-ageotype – markers associated with cardiac stress, lipid handling and inflammatory patterns that indicate cardiovascular aging.
- Metabolic-ageotype – disturbed lipid and small-molecule metabolism patterns that suggest higher metabolic age.
- Immune-ageotype – elevated inflammatory cytokines and patterns that indicate immune aging.
Why this matters: if your metabolomics suggests a metabolic ager pattern you target diet, exercise and metabolic-focused therapies. If you have a cardio ager pattern you focus on lipids, blood pressure and cardio-specific interventions. The actionable value of agotypes is that they give targeted recommendations instead of a generic “you are older biologically” number that does not tell you what to change.
One vendor I use for metabolic profiling offers dried blood spot metabolomics with 650 metabolites and AI-driven recommendations. The kit is mailed in, and results can be integrated into personalized plans. Micro-sampling technologies have evolved over the last decade to permit meaningful metabolomic and proteomic readouts from small volume samples when handled and processed properly.
Whole-body MRI and the value of baselines
Whole-body MRI or targeted imaging can detect early organ-level abnormalities long before symptoms. The practical value of an initial high-quality baseline scan is that it gives you a starting point. If a lesion or nodule is detected later you can rapidly determine if it is new or stable. Many physicians are concerned about overdiagnosis from very sensitive imaging, but I believe the baseline-first approach reduces downstream overreaction and helps prioritize real changes over benign static findings.
Typical use-cases
- Baseline whole-body MRI for high-risk individuals – history of familial cancers, significant family cardiac disease, or personal high-risk genetics.
- Follow-up imaging to track nodules rather than immediate invasive steps for small, stable lesions.
Air quality, environmental monitoring and health
Environmental exposures matter. Particulate matter, pesticides, DEET and volatile organic compounds are measurable and frequently correlated with inflammation, respiratory symptoms and longer-term chronic disease risk.

Steps I take and recommend
- Measure your indoor air quality with a portable monitor that records PM2.5, PM10 and volatile organic compound indicators. Keep a small device on or near your workspace and in the bedroom to log typical exposures. The numbers help you objectively decide whether to ventilate, filter or avoid a location.
- Use an air purifier with HEPA filtration if PM2.5 or PM10 routinely exceed healthy thresholds. For wildfire smoke, use a high-efficiency purifier and keep windows closed until outdoor air clears. Typical target values: PM2.5 less than 12 micrograms per cubic meter when possible; values above 35 indicate moderate to unhealthy air.
- Test household water for contaminants if you live in a region with industrial agriculture or aging infrastructure. Use a filtered glass bottle for daily drinking and avoid single-use plastic bottles when possible.
- Avoid unnecessary DEET exposure and routine topical insecticide use indoors. If working in agriculture or rural settings, use protective practices and ask for environmental testing when feasible.
Wearables, HRV, mindset and what to measure daily
Wearables provide continuous physiological streams that are useful when paired with periodic lab-based measures. The most reliable wearable-derived metrics I use:
- Resting heart rate – general cardiovascular fitness marker.
- Heart rate variability (HRV) – index of autonomic balance. Lower HRV commonly seen during illness, stress and sleep deprivation.
- Sleep stages – wearable algorithms vary, but trends are useful. Stationary sensors like mattress covers can be more accurate for staging than wrist devices for some people.
Simple HRV practice I recommend
- Periodically do a long controlled exhale technique to stimulate vagal tone: inhale comfortably, then perform a slow, complete exhale to empty the lungs, hold for a second or two then inhale. Repeat 5 times. Short practice multiple times per day raises baseline HRV in many people.
- Use HRV trends as a decision guide for training intensity and recovery. If HRV drops substantially and does not recover within a few days, reduce intensity until it stabilizes.
Mindset and sleep tip
Anticipation of positive events the next day improves sleep quality. Cultivate small rituals or positive anticipatory elements before sleep to boost sleep depth and REM proportion when time permits.
Acupuncture and somatic interventions
Integrative interventions like acupuncture have mechanistic plausibility and randomized evidence in several domains. Electroacupuncture can produce cardiovascular and immune effects via vagal pathways and splenic signaling. My experiential notes:
- I participated in an electroacupuncture blood-pressure targeted protocol and observed a meaningful reduction in systolic blood pressure after the session and maintained across several sessions. Individual results vary but the physiologic magnitude can be clinically meaningful for selected responders.
- Acupuncture likely works via nervous system modulation of immune and autonomic pathways; needle placement patterns matter.
If you try acupuncture
- Use licensed practitioners.
- Ask whether they use electroacupuncture for cardiovascular targets.
- Track blood pressure and other metrics objectively before and after to determine whether you are a responder.
Mental health, immersive interventions and measurable outcomes

Group-based immersive psychological interventions can yield durable improvements in mood, anxiety and well-being. For larger, well-run immersive programs researchers have measured improved survey scores and in pilot projects also measurable reductions in inflammatory markers. The core features that matter:
- High intensity, high structure – a multi-day immersive that includes breathwork, somatic work and cognitive reframing can catalyze behavioral change.
- Follow-through – participants who keep practicing techniques learned during the immersive (breathwork, journaling, evening routines) show the most durable benefits.
- Measurement – pre/post surveys, wearables and laboratory markers help objectify benefit. I recommend one-month, three-month and six-month reevaluations to track sustainability.
Micro-sampling and single-drop blood metabolomics
Advances in dried blood spot metabolomics and proteomics allow high-resolution biochemical phenotyping from small capillary samples if the sampling method preserves analyte stability. What this enables:
- High-frequency sampling over weeks without phlebotomy.
- Tracking metabolic fluxes across sleep-wake cycles and food intake.
- Correlating blood-level small molecules and proteins with wearable physiological data and environmental exposures to build actionable insights.
Operational tips
- Use validated kits and labs with rigorous mass spectrometry pipelines.
- Coordinate sampling windows with your clinician or protocol team to ensure interpretable patterns.
FAQ - answers I give most often
Q: How long should I wear a CGM the first time?
I recommend 10-14 days. That duration captures weekday and weekend behavior, multiple meals and gives a robust picture of typical glucose variability. Use the data to learn which foods cause prolonged spikes for you and to measure the effect of post-meal walks and resistance training.
Q: Which fiber should I take first?
If you have elevated LDL or ApoB psyllium-type fiber is a logical first trial. Dosing: start 5-10 grams daily and titrate to 10-30 grams daily as tolerated. If you are testing inulin, start at 2-5 grams and increase slowly to 10 grams to minimize bloating. Track CRP and LDL to determine effect.
Q: What sleep supplements are safest to try first?
Start with glycine 3 grams nightly or L-theanine 100 mg nightly. Both are well tolerated by most people and have mild support for sleep depth and calm. Magnesium threonate works for many but adjust dose based on bowel tolerance and elemental magnesium content.
Q: I take GLP-1 drugs and lost weight quickly. How do I prevent muscle loss?
Prioritize resistance training 3-6 times per week, ensure daily protein intake of ~1.2-1.6 grams per kilogram if clinically appropriate, and maintain progressive loading when possible. If you are losing strength or muscle mass unexpectedly, consult your prescribing clinician and a sports medicine or exercise physiologist to refine programming and nutrition.
Q: Are single drop metabolomics accurate?
Yes, when performed by validated labs with quality control and proper sampling kits. The stability of analytes depends on the sampling card and the storage method used. Use established vendors with published validation data.
Q: Should I try acupuncture for blood pressure?
For some people acupuncture or electroacupuncture produces clinically meaningful reductions in blood pressure. If you have high blood pressure and medications are not fully controlling it, discussing a short acupuncture course with a qualified practitioner and tracking ambulatory or home blood pressure is reasonable under clinician supervision.
Closing: a pragmatic invitation
Personalization of metabolic health is no longer theoretical. The tools are available: CGMs, validated wearables, dried blood spot metabolomics, fiber-specific trials and environmental sensors. The core habit that yields the most return is the measurement-habit. Measure, change one variable, measure again. Iterate. This turns guesswork into reproducible change. For readers ready to put this into practice with structured guidance, check out our Integrate program.
Measure more, guess less. The short-term work of measurement and iteration yields long-term gains in healthspan.