Today we’re taking a closer look at the Yuka app, a tool that many people turn to when trying to make healthier food choices. The app promises quick, visual answers about whether a product is healthy or not, but when you dig deeper, the reality is more complicated. Some of Yuka’s insights can be helpful, some are neutral, and others could even be harmful if followed without personalization, especially for those rebuilding health after cancer.
One of Yuka’s best features, however, is its ability to flag additives and preservatives you might not realize are hiding in everyday foods. This can be eye-opening and help you spot ingredients that may undermine your health goals, especially if you’re trying to reduce your exposure to unnecessary chemicals.
In this post, we’ll walk through exactly how Yuka scores foods, highlight where those scores make sense, and point out where they fall short. Using real examples like cottage cheese, canned tuna, and protein bars, we’ll show why a one-size-fits-all app can’t replace individualized nutrition planning. Most importantly, we’ll share practical strategies you can use instead of relying blindly on an app along with clear, evidence-informed guidance on supplements, dosage ranges, and protocols that support true recovery and resilience. Let’s explore what the research says, where Yuka gets it right, and how you can take a smarter, more personalized approach to your health journey.
Table of Contents
- Why I Evaluated Yuka
- How Yuka Works: The Scoring System Explained
- Caveat: The App Was Not Designed for Cancer Survivors
- Example 1: Cottage Cheese
- Example 2: Canned Tuna
- Example 3: Protein Bars
- How to Use Yuka Safely If You Choose To Use It
- Practical Food Strategies For Cancer Survivors
- Supplements and Exact Dosages I Recommend in Recovery
- Personalizing Your Nutrition Plan
- Practical Shopping and Meal Strategies
- When To Get Professional Help
- FAQ
- Final Thoughts
Why I Evaluated Yuka
Yuka is popular because it is simple. Point your phone at a barcode and get a single numerical score plus a color code green, yellow, or red. People like simple. Cancer survivors in particular are trying to do everything they can to reduce recurrence risk and to support recovery after treatment. When you re exhausted and overwhelmed, an app that looks like it will tell you what to eat is alluring. But nutrients, recovery, and cancer risk are not black and white. When a tool that was designed for the general population gets repurposed as an on the spot cancer nutrition guide, problems arise.
I evaluated Yuka because I want you to make informed choices, not fearful or rigid choices. If you are rebuilding your health after cancer, your food choices must be targeted, individualized, and evidence informed. Yuka s scoring system mixes validated methods with app specific rules that are not backed by strong clinical evidence for people recovering from cancer. That mix can lead to unnecessary avoidance of beneficial foods, and in some cases trigger real anxiety about everyday eating.
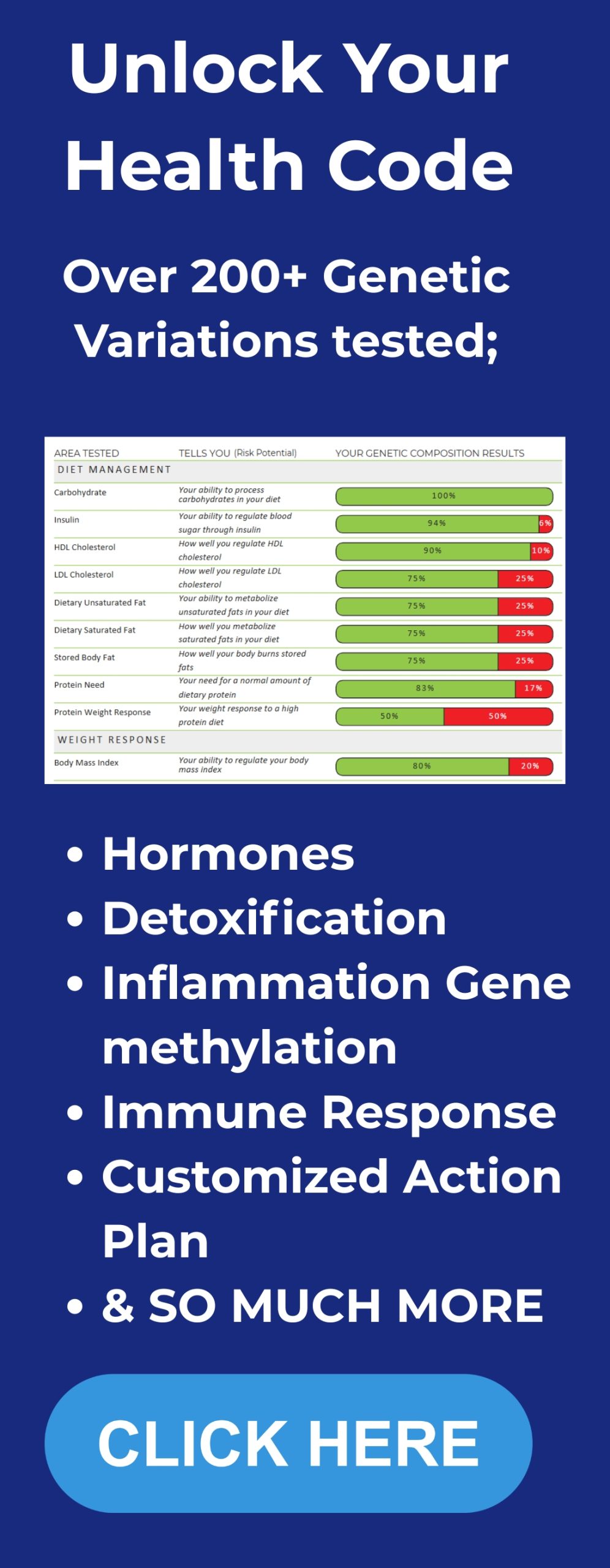
How Yuka Works: The Scoring System Explained
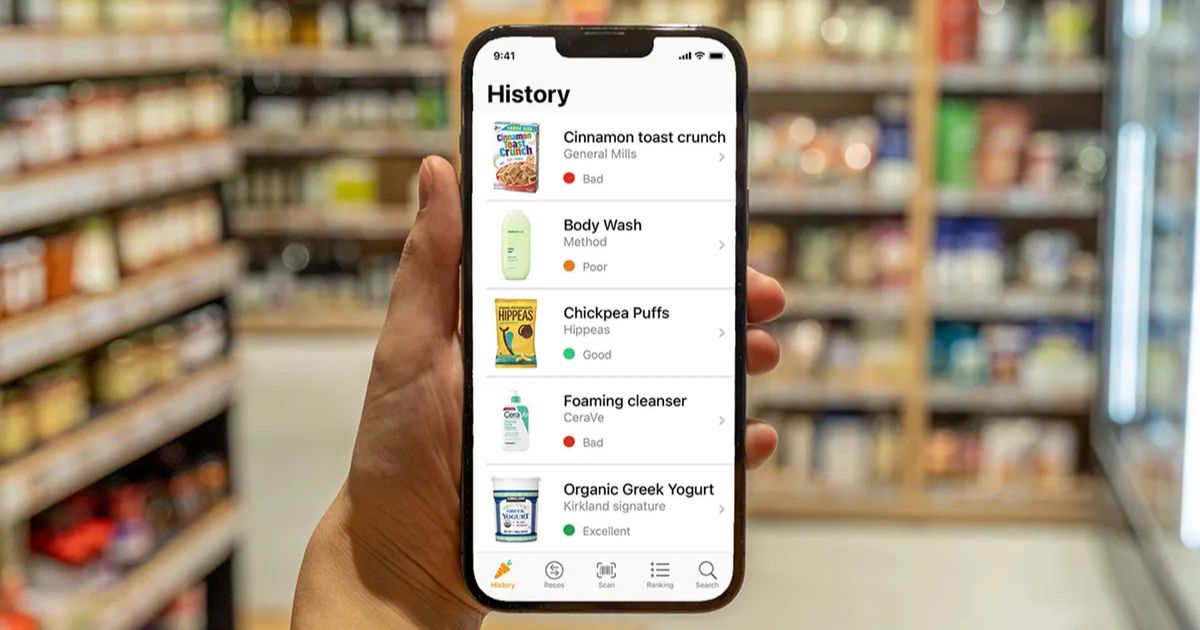
Image source: Fox News
Yuka reports a score out of 100 for food and cosmetic products. It presents that score with an A to E grade and color coding: green for go, yellow for caution, red for stop. It breaks the scoring down into three components:
- Nutritional quality about 60 percent of the score. Yuka uses NutriScore methodology here. NutriScore is a front of pack label that originated in Europe and assigns A through E grades based on calories, sugar, saturated fat, sodium, fiber, protein, and fruit, vegetable, and nut content.
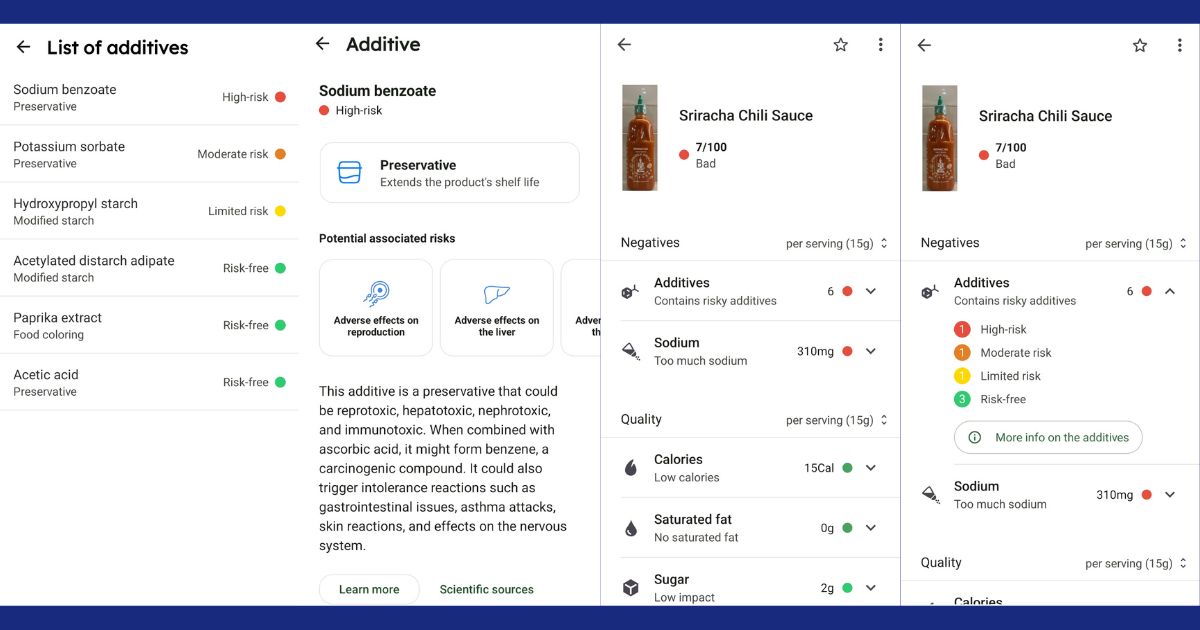
- Additives about 30 percent of the score. Yuka maintains a catalog of additives it flags as problematic. For some additives they cite studies, for others they use a precautionary approach.
- Organic certification about 10 percent of the score. Organic status slightly boosts a product s score in Yuka.
On the surface this looks reasonable. The NutriScore element is evidence based and aligns with public health efforts to make it easier to compare packaged foods. The problem comes from two sources. First, the additive and organic weighting represent a one size fits all value judgement that is not necessarily relevant to cancer survivors. Second, Yuka s interpretation of scientific evidence behind some additives is selective. In other words, Yuka sometimes classifies an additive as unsafe on the basis of preliminary animal or in vitro studies while ignoring regulatory conclusions or human data that do not support a risk.
Caveat: The App Was Not Designed for Cancer Survivors
One of the most important principles I emphasize with clients is that cancer recovery nutrition must be targeted. Your diagnosis, your treatment history, your current body composition, your labs, and your goals all matter. Yuka was designed for the general public to assess the relative healthfulness of packaged products. That is fine for simple public health messaging, but it becomes dangerous when people assume a low Yuka score means an item increases cancer risk or must be avoided at all costs.
Consider this essential point. A product receiving a negative flag on Yuka may be high in additives or not organic, but that does not automatically translate to increased cancer risk or poor outcomes for an individual survivor. Conversely, a green score does not replace tailored attention to nutrients you may need more of after treatment, such as high quality protein or healthy fats. If you make the mistake of letting the app decide for you, you may miss nutritional opportunities that matter for long term recovery.
Example 1: Cottage Cheese
Let s go through a detailed example so you can see how Yuka’s logic works and where it breaks down. I scanned a commonly available cottage cheese and Yuka returned a score of 45 out of 100. It showed a yellow light and classed the product as poor. That feels alarming if you re a cancer survivor looking for safe dairy and affordable protein. But what drove that poor score?
Yuka flagged the presence of an emulsifier called polysorbate. The app described polysorbates as agents that might disrupt gut microbiota and could be linked to autoimmune issues. Yuka supported the claim with three references: two mouse studies and a published gut simulation model. On top of that Yuka also highlighted some regulatory discussion, but used animal data to argue that the additive raises concerns.

Here is my assessment.
- The concern raised by Yuka about polysorbates is not evidence of human harm at typical dietary exposure. Two animal studies and an in vitro or simulation model are useful as hypothesis generating tools. They are not definitive evidence that a food additive at the dose found in cottage cheese causes autoimmune disease in humans or increases cancer risk.
- Regulatory bodies such as the European Food Safety Authority evaluate both animal data and human exposure levels to set acceptable daily intakes. For many emulsifiers currently in use, EFSA and other regulators have not identified human safety concerns at the levels normally consumed.
- Yuka s presentation weighs the additive concern heavily and visually emphasizes it with red icons, making it the dominant takeaway even when the product performs well on other measures.
Why does this matter? Because cottage cheese has meaningful nutritional benefits for most cancer survivors. It is often high in protein, low calorie, and low in saturated fat. For many women recovering from breast cancer and for other survivors, maintaining lean mass and avoiding excess fat, particularly saturated fat, are important. Additionally, cardiovascular health is a central long term consideration, especially for breast cancer survivors, since heart disease is a leading cause of death in many survivor populations. Avoiding a high quality protein like cottage cheese solely because an app flags a hypothetical additive risk could lead to unnecessary protein loss, reduced recovery, and poorer outcomes.
In short, I recommend looking past the red icon and evaluating the full nutritional context. If you have specific immune or digestive issues, discuss them with your oncology dietitian or medical team. But for most survivors, cottage cheese remains a useful, inexpensive way to boost protein and keep calories in check.
Practical steps when you encounter a flagged additive
- Check the regulatory status. See if EFSA, FDA, or Health Canada has assessed the additive and what their conclusion was regarding typical dietary exposure.
- Look for the dose. If the supporting references are animal studies, see whether the doses used were realistic compared to human intake. Often animals get very high doses that are not comparable.
- Weigh benefits and risks. If a food provides a major nutrient you need, it may be preferable to keep it rather than swap it for a lower quality substitute.
- If you remain concerned, aim for alternatives without the additive, but avoid creating rigid rules that eliminate entire food groups without good reason.
Example 2: Canned Tuna
Canned tuna scored 78 out of 100 on Yuka and received a green light. The app highlighted the positives: high protein, low calories, and no additives. It noted one negative: somewhat high sodium in some preparations. I largely agree with this assessment with an important caveat.
Tuna is a convenient source of lean protein and omega 3 fatty acids, and it can be an excellent option for survivors who need to increase protein intake without adding a lot of saturated fat. I often recommend canned fish as part of a balanced approach because it is shelf stable, cost effective, and nutritionally dense.

However, two cautions apply:
- Mercury exposure Larger predatory fish such as albacore or bigeye tuna can have higher mercury levels. For women of childbearing potential or others with specific exposure concerns, I recommend limiting albacore tuna to a couple of servings per week and prioritizing light tuna if you eat it frequently. Your local public health guidance can help quantify safe intake limits.
- Sodium and preparation Some canned tuna is packed in brine or contains added salt. If you re watching sodium intake for blood pressure or heart health, choose tuna packed in water with no added salt or rinse brined tuna briefly.
On balance I find Yuka s positive assessment of canned tuna aligns with the needs of many survivors. The app s lack of additive flags is accurate because pure tuna does not require emulsifiers or preservatives. Still, always read the label for sodium and choose light tuna more often if you are worried about mercury.
Example 3: Protein Bars
Protein bars are a frequent target of Yuka and similar scanning apps. I scanned a typical commercially available protein bar and Yuka returned a low score 27 out of 100 with a red light. Yuka s primary complaints were that the bar was too caloric and that it contained sucralose, which the app flagged as potentially hazardous based on selective interpretation of epidemiological data.

This is an important area to unpack because many survivors rely on protein bars for convenient nutrition on the go. For some women recovering from treatment, increasing protein intake is essential to rebuild muscle mass. Calorie content alone is not a reason to avoid a food if you need those calories and proteins for recovery.
Here is what I recommend you consider:
- Individualize calorie targets If you are actively rebuilding lean mass or have a poor appetite post treatment, a protein dense bar with 200 to 300 calories and 15 to 25 grams of protein could be a very useful tool. Yuka s blanket flag of “too caloric” assumes a baseline caloric need that does not exist for everyone.
- Look beyond the sweetener headline Yuka flagged sucralose and cited the NutriNet Sante study. The NutriNet Sante cohort has produced important observational findings, but when data are controlled for body weight and other confounders, the association between sucralose and cancer risk does not persist. The larger body of evidence, including expert consensus, does not support a causal relationship between sucralose at typical dietary levels and increased cancer risk in humans.
- Check the overall ingredient quality For bars I prefer whole food ingredients, minimal sugar alcohols if you have GI sensitivity, and a balance of protein and healthy fats to support satiety and recovery. Avoid bars that are primarily cheap carbohydrate fillers with minimal protein.
Bottom line if you need the calories and protein, a well chosen protein bar can be an asset. Yuka s generic scoring can create unnecessary fear, especially when calories are flagged as a negative without context.
How I Use It Personally
I don’t just analyze Yuka from a professional standpoint. I’ve also used it myself to see how it stacks up in real life.
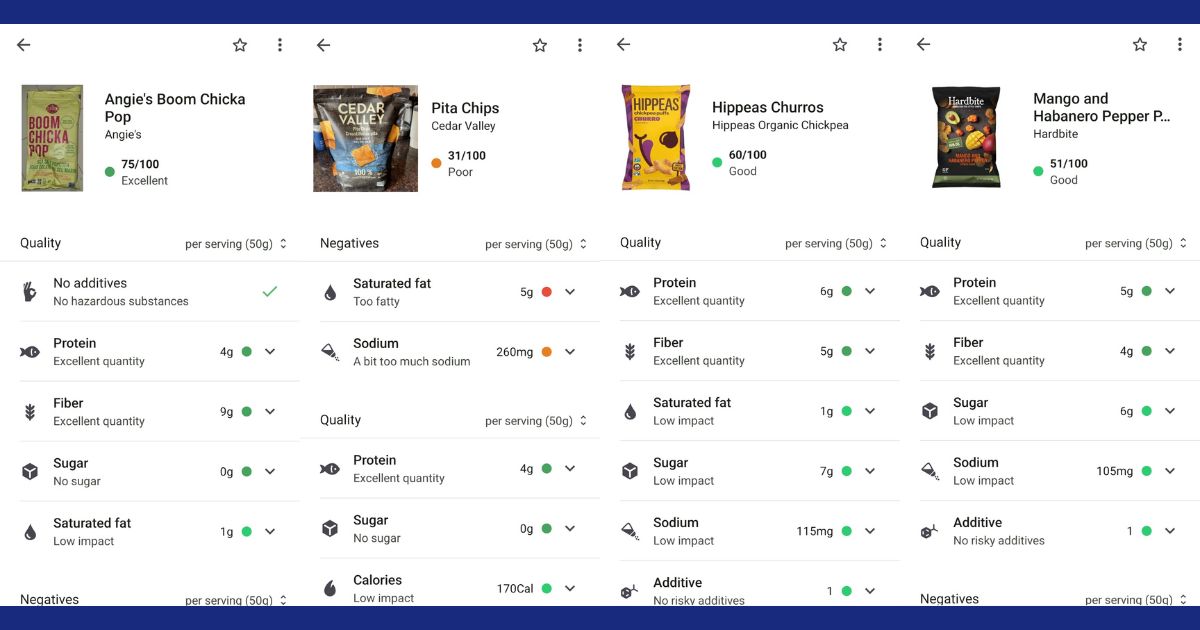
For example, chips. We all get cravings, and when I do, I’ll scan a few options. Some come back with warnings for higher sodium or fats. Honestly, that doesn’t bother me too much when I’m treating myself. What matters more to me is whether the chips are free from questionable preservatives or additives that don’t need to be there. If I’m going to indulge, I want it to be as clean as possible.
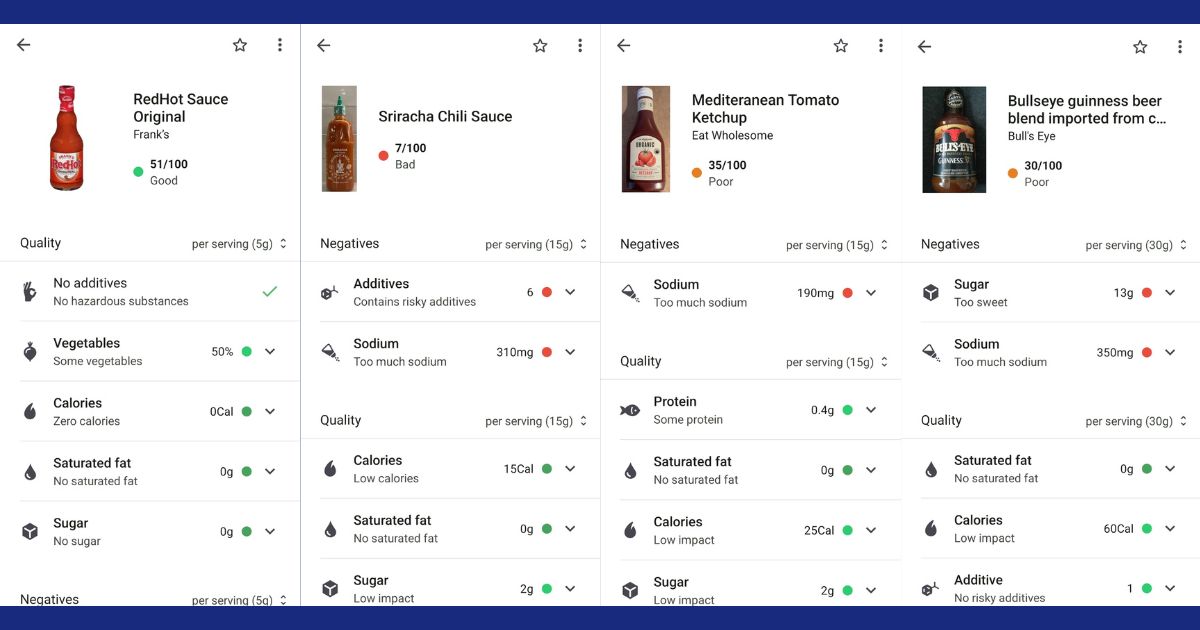
Then there are sauces. Oh, sauces. I almost cried the first time I scanned Sriracha and saw how low it scored even though it’s relatively low in sugar. Why the harsh rating? Turns out, Yuka flagged it for the preservatives it contains. That was frustrating to see because I love it. At least Frank’s RedHot came back with a much better score.
Curious, I dug deeper into the Sriracha issue. The “bad” rating wasn’t about sugar or calories at all — it was because of the preservatives on the ingredient list. That’s what Yuka really penalized. While some of those additives may not be truly hazardous at everyday levels, it was eye-opening to see just how much the app weighs those ingredients in its scoring.
How to Use Yuka Safely If You Choose To Use It
If you like Yuka for convenience, there are ways to use it that minimize harm and maximize utility. Here are practical rules I suggest:
- Use Yuka as a first pass for comparing similar packaged items. If you re choosing between two flavored yogurts, Yuka can highlight differences in sugar and additives that matter at the margin.
- Always dig into the reasoning behind a red flag. Check whether the evidence is animal based, in vitro, or human observational. Consider the dose and whether regulatory agencies have identified a risk at typical exposures.
- Prioritize clinical context. If you need protein and a Yuka flagged product contains valuable protein, do not discard it without a conversation with your oncology team or dietitian.
- Keep a balanced perspective. If multiple foods you enjoy are flagged, create a plan with an oncology informed dietitian to replace items sensibly, rather than eliminating whole categories overnight.
- If using Yuka increases anxiety, stop using it. Trust your clinical team and a personalized nutrition plan instead.
Practical Food Strategies For Cancer Survivors
Outside of an app, here are the concrete food strategies I use with clients that have a stronger evidence base for supporting recovery and lowering recurrence risk when combined with other lifestyle changes like physical activity and smoking cessation.
- Prioritize high quality protein Aim to distribute protein intake across the day. For many survivors I work with, a target of 1.0 to 1.5 grams of protein per kilogram of body weight per day helps preserve or rebuild lean mass. For example, a 70 kilogram person might aim for 70 to 105 grams of protein daily. Focus on lean meats, poultry, fish, dairy, eggs, tofu, tempeh, legumes, and supplemental protein when needed.
- Choose healthy fats Include sources of omega 3 fatty acids such as salmon, mackerel, sardines, or a high quality fish oil supplement if recommended. Replace excess saturated fat with unsaturated fats found in nuts, seeds, avocados, and olive oil.
- Vegetables and fiber Aim for a variety of colorful vegetables and adequate fiber intake. Fiber supports gut health and metabolic regulation.
- Limit ultra processed foods Where possible, minimize intake of highly processed products with long ingredient lists and added emulsifiers and fillers. This is a flexible guideline, not an absolute rule. Occasional convenience foods can be fine if they help adherence and prevent calorie deficits or excessive stress.
- Hydration and sleep These often get overlooked but support recovery and metabolic health.
Supplements and Exact Dosages I Recommend in Recovery
Now I will share clear guidance on supplements, including exact doses I commonly recommend as part of a recovery plan. Before you read further, please note three important safety points.
- Supplements are not a substitute for a whole food first diet and medical care.
- Always discuss supplements with your oncology team. Some supplements can interact with medications or treatments and some are contraindicated during active chemotherapy or radiation.
- I am providing typical evidence informed doses used in recovery protocols. Individual needs vary based on lab testing, body weight, medication interactions, kidney and liver function, and other factors.
I work with survivors to personalize dosing. These are my starting points I frequently use while monitoring labs and symptoms.
Vitamin D3
Why I use it. Vitamin D is widely deficient and plays roles in immune function, bone health, and potentially cancer prognosis. Here’s why you may need more Vitamin D. Many survivors are deficient after treatment.
Typical dose. For most survivors I start with Vitamin D3 2000 to 5000 international units per day orally. If labs show deficiency 25 hydroxyvitamin D below 20 nanograms per milliliter or 50 nanomoles per liter, I often use a repletion strategy such as 50 000 international units once weekly for 6 to 8 weeks under medical supervision, then move to maintenance dosing of 2000 to 4000 international units per day. Target serum 25 hydroxyvitamin D between 30 and 50 nanograms per milliliter or 75 to 125 nanomoles per liter.
Monitoring. Check serum 25 hydroxyvitamin D, calcium, and kidney function before high dose repletion and periodically during maintenance. Adjust dose based on levels.
Omega 3 Fish Oil
Why I use it. Omega 3 provide anti inflammatory effects, support cardiovascular health, and help with muscle preservation. They are particularly useful if dietary seafood intake is low.
Typical dose. I commonly recommend 1000 to 2000 milligrams per day of combined EPA plus DHA. For individuals with elevated triglycerides or significant inflammation, doses up to 3000 to 4000 milligrams per day under physician supervision can be used. Choose a purified product that is third party tested for contaminants including mercury and PCBs.
Monitoring. Watch for bleeding risk if you take anticoagulant medications. Always inform your physician if you re using higher doses.
Magnesium
Why I use it. Magnesium supports muscle function, sleep, and many enzymatic processes. It also helps mitigate some treatment related neuropathy and sleep disturbances in certain cases.
Typical dose. Magnesium glycinate or magnesium citrate 200 to 400 milligrams daily is a commonly tolerated maintenance dose. Since not all magnesium forms work the same, it’s important to choose wisely — learn why here. For those wanting a trusted source, we often recommend CanPrev’s Magnesium. If constipation is a problem, magnesium citrate at the lower end may help. Spread dosing across the day if higher doses are used. Avoid high doses above 400 milligrams per day without medical guidance if you have impaired kidney function.
Probiotic
Why I use it. A healthy microbiome supports digestion and immune modulation. Many survivors experience antibiotic exposure during treatment and may benefit from probiotic repletion.
Typical dose and strains. I typically recommend a multi strain probiotic providing 10 to 50 billion colony forming units per day, including strains such as Lactobacillus rhamnosus, Bifidobacterium longum, and Lactobacillus acidophilus. Use a reputable brand that guarantees strain identity and potency. Take probiotic away from antimicrobial medications and discuss timing if you are on active immunosuppressive therapy.
Vitamin B12
Why I use it. B12 deficiency is common in older adults and those with altered GI function. Symptoms include fatigue, neuropathy, and cognitive changes.
Typical dose. If serum B12 is low or borderline, I often start with methylcobalamin 1000 micrograms daily sublingually for a month, then reassess. For clear deficiency, intramuscular B12 injections 1000 micrograms once a week for 4 to 6 weeks and then monthly may be used. Some people remain on 1000 micrograms daily sublingual maintenance.
Monitoring. Check serum methylmalonic acid if diagnosis is unclear. Adjust based on lab response and symptoms.
Multivitamin
Why I use it. After treatment many patients have gaps in micronutrients due to poor appetite, altered absorption, or dietary restriction.
Typical dose. A well balanced multivitamin with minerals taken daily is a reasonable baseline. Choose a product that does not contain mega doses of single nutrients. Look for one that provides 100 percent of most B vitamins, 100 percent of vitamin C, vitamin A in retinol or provitamin forms within recommended ranges, and minerals such as zinc and selenium in moderate amounts. Avoid high dose antioxidant supplements during active treatment without oncologist approval.
Vitamin C
Why I use it. Vitamin C is important for immune health and connective tissue repair. High dose intravenous vitamin C is sometimes explored in integrative settings and requires medical supervision. Oral vitamin C is generally safe at moderate doses.
Typical dose. Oral vitamin C 500 to 1000 milligrams daily is a common maintenance dose. If you have a history of kidney stones or iron overload, discuss with your physician before high dose oral or IV use.
Curcumin and Other Phytonutrients
Why I use it. Curcumin has anti inflammatory properties but oral absorption is limited. It can be useful as a dietary phytonutrient in combination with a healthy diet.
Typical dose. If used as a supplement, curcumin with bioavailability enhancement 500 to 1000 milligrams per day is a common range. Avoid during active chemotherapy unless cleared by your oncology team because of potential interactions.
Final safety note on supplements. Supplements can be helpful when used appropriately, but they are not without risk. Interactions with hormonal therapies, chemotherapy agents, anticoagulants, and other medications are possible. I always advise a thorough medication review before adding any new supplement.
Personalizing Your Nutrition Plan

Generic advice is the enemy of good recovery planning. Here is the step by step approach I use with clients and that you can adapt for yourself or discuss with your medical team.
- Baseline assessment. Review your treatment history, current medications, lab values including vitamin D, B12, iron studies, thyroid and metabolic panel, and body composition goals. You can also go deeper with personalized DNA insights to see how your genetics influence nutrient needs and recovery.
- Set priorities. If your main concerns are muscle loss and fatigue, prioritize protein and energy. If you are overweight with cardiometabolic risk, set a regime that supports weight loss with attention to preserving muscle mass.
- Food first. Aim to meet most nutrient needs through whole foods, using supplements to fill gaps identified by labs or clinical symptoms.
- Monitor and adjust. Recheck labs at intervals, track symptoms, and adjust supplement doses and food patterns based on response.
- Psychological health. Include mental health support for struggles with anxiety about food, body image, or fear of recurrence. Disordered eating can develop after cancer and is treatable with professional help.
Practical Shopping and Meal Strategies
Here are the hands on tips I give people who are trying to apply evidence based nutrition without getting lost in app scores.
- Focus on protein at every meal. Examples: Greek yogurt or cottage cheese at breakfast, a salad topped with tuna at lunch, and a portion of salmon or a chicken breast at dinner.
- Use canned and frozen produce to reduce cost and waste while keeping nutrition high.
- Read the ingredient list. Short ingredient lists with recognizable items are usually better than long lists of industrial additives.
- Plan meals around vegetables and a quality protein first. Add whole grains or legumes as needed for energy and fiber.
- When buying packaged foods, use apps like Yuka as one data point only. Don t let a single score override your clinical context.
When To Get Professional Help
If any of the following apply, seek an oncology trained dietitian or your medical team before making changes based on an app.
- You are currently receiving chemotherapy, immunotherapy, or radiation.
- You have ongoing significant weight loss or weight gain despite attempts to adjust intake.
- You have symptoms of malabsorption, severe gastrointestinal issues, or significant neuropathy.
- You find that food apps trigger anxiety, rituals, or obsessive behaviors around eating.
- You are considering high dose supplements or intravenous therapies.
FAQ
Is Yuka dangerous for cancer survivors?
Yuka itself is not inherently dangerous. However, when used without context it can encourage unnecessary avoidance of nutritious foods and create anxiety. The app s emphasis on additives and organic status may not reflect the specific nutrition priorities of survivors. Use it cautiously and always discuss major changes with your oncology team.
Should I stop using Yuka?
Not necessarily. If you use it as a comparison tool to choose between similar packaged foods and you remain grounded in a personalized nutrition plan, it can be helpful. If you find it promotes worry or rigid eating, stop using it.
Are additives like polysorbates proven to cause cancer in humans?
No. Most of the studies cited to raise concern are animal or in vitro models. Regulatory agencies evaluate these data and human exposure levels before flagging risks. At typical dietary levels, many emulsifiers and additives have not been shown to cause cancer in humans. That said, research continues, and I encourage staying informed through reputable sources and discussing concerns with clinicians.
What should I do if Yuka flags a food I rely on?
Investigate the reason for the flag. Is it calorie content, sodium, an additive, or low NutriScore due to sugar/saturated fat? Consider the food s benefits. If it provides needed protein or nutrients, keep it and discuss any long term alternatives with a dietitian. Avoid abrupt elimination without a plan.
Which supplements do you recommend and at what doses?
Common supplements I use in recovery include Vitamin D3 2000 to 5000 international units per day with repletion doses if deficient, omega 3 fish oil 1000 to 2000 milligrams per day of combined EPA DHA, magnesium 200 to 400 milligrams per day, a probiotic providing 10 to 50 billion CFU per day, Vitamin B12 1000 micrograms per day sublingually if low or intramuscular replacement if deficient, and a balanced multivitamin. Always discuss with your medical team before starting supplements.
Can sucralose increase cancer risk?
The current body of evidence does not support a causal relationship between sucralose at typical dietary doses and cancer in humans. Observational studies may show associations that vanish when adjusting for confounders like body weight. If you prefer to avoid artificial sweeteners, that is a valid personal choice, but the evidence does not mandate avoidance for cancer prevention in most cases.
How do I evaluate evidence when an app cites studies?
Ask these questions: Are the studies in humans or animals? If in animals, were the doses comparable to human consumption? Are there large, well designed human studies or meta analyses? What do regulatory agencies say? If you are unsure, consult an oncology trained dietitian or clinician.
Final Thoughts
Yuka is a useful tool for quick comparisons, but it is not a substitute for individualized cancer recovery nutrition. The app mixes evidence based approaches like NutriScore with app specific additive judgments that may exaggerate risk. For survivors, the most important elements of nutrition are clarity on protein needs, restoration of metabolic health, support for cardiovascular function, and prevention of disordered eating patterns. If a tool increases worry, avoid it.
Use Yuka when it helps you choose between packaged options, but prioritize clinical context and lab guided supplementation when rebuilding your health. If you want a structured, personalized plan that includes food, lifestyle, and evidence informed supplements, my colleagues and I can provide practical protocols tailored to recovery after cancer. Learn how we can integrate everything into one actionable plan.
If you have questions about specific products you use, specific supplement combinations, or need help interpreting lab results, reach out to a clinician experienced in survivorship care. Nutrition matters deeply during recovery. Use tools wisely and protect your peace of mind while you build resilience and long term health.