Today we’re diving into an important topic that affects health and longevity more than most people realize: alcohol. For years it has been framed as a harmless social ritual, a way to relax, or even a reward at the end of the day. But the science paints a very different picture. Alcohol is not a benign indulgence; it has measurable effects on the brain and body that accumulate over time and directly work against long-term health and vitality.
In this post, we’ll explore why alcohol is so damaging in both the short and long term, what the latest research reveals about its impact, and how removing it can unlock profound improvements in energy, focus, and resilience. You’ll also learn practical, evidence-based strategies to reduce or eliminate alcohol use, plus targeted nutrition and supplement protocols to help support recovery and build lasting health.
If you’re ready to understand exactly why alcohol holds so many people back, and discover the tools to move beyond it, let’s take a closer look at what the science really says.
Table of Contents
- Why I Say Alcohol Is a Longevity Killer
- The Immediate Hit: Hydration, Hormones, and Cognitive Fog
- Long-Term Consequences: Liver, Brain, Cancer, and Sleep
- Social Pressure, Habits, and the Hidden Costs
- Benefits of Eliminating Alcohol: What You Can Expect
- How to Cut Alcohol Out: Practical, Stepwise Plan
- Targeted Supplements and Nutrition Protocol: What I Recommend and Why
- How to Implement This Protocol Safely
- Behavioral Tools That Amplify Success
- Common Questions I Get and Practical Answers
- My 8-Week Action Plan
- FAQ
- Final Thoughts: Small Changes, Big Results
Why I Say Alcohol Is a Longevity Killer
This is not fear-mongering. It is a synthesis of hard science and practical experience. Alcohol is one of the top five causes of chronic disease worldwide. It’s classified as a Group 1 carcinogen and is directly linked to multiple cancers, liver disease, impaired brain health, sleep disruption, and metabolic damage. When you add up how alcohol affects sleep, cognition, inflammation, liver function, and cancer risk, the case becomes clear: regular alcohol use chips away at your health span and likely shortens your lifespan.
Most people focus on the immediate buzz or the idea that “a glass of wine is healthy.” The short version of what I want to convince you of is this: the immediate effects are only the starting point. Daily or weekly alcohol intake compounds over years and decades, accelerating biological aging, impairing repair systems, and increasing risk for serious disease. Below, I break it down into the key systems alcohol harms and why those systems matter for longevity.
The Immediate Hit: Hydration, Hormones, and Cognitive Fog
Let’s start with immediate effects because they are the ones you notice first and because they already give you a preview of what happens over time.
Alcohol Dehydrates You and Disrupts Hormone Balance
Alcohol inhibits the release of antidiuretic hormone, ADH, which normally tells your kidneys to conserve water. With ADH suppressed, you urinate more and lose more fluid. That is why hangovers often feel like dehydration. But it is more than thirst. Dehydration impairs circulation, reduces nutrient delivery to tissues, raises perceived exertion during exercise, and increases systemic stress.
When dehydration becomes regular, your body is constantly compensating. Chronic mild dehydration shifts electrolyte balance, can interact with blood pressure control, and makes sleep and recovery worse. The next time you wake up sluggish and foggy after drinking, realize that the dehydration mechanism is only the first effect in a cascade.
Mental Fog, Slower Reaction Times, and Impaired Learning
Alcohol impairs cognitive processing for up to 24 hours, even after blood alcohol levels return to zero. Reaction time, memory consolidation, attention, and executive function are affected. Research shows reduced brain activity in areas responsible for learning and memory after alcohol use, and these effects become more pronounced with repeated exposure.
If you’re trying to perform at work, learn a new skill, or optimize your day, alcohol sabotages those goals. One drink may not ruin your week, but regular drinking reduces the amount of high-quality, productive time you have. Over months and years, that lost productivity translates into reduced personal growth and diminished capacity to engage in the habits that increase longevity.
Long-Term Consequences: Liver, Brain, Cancer, and Sleep
Over weeks, months, and years, the cumulative impact of alcohol becomes much more serious. The liver, brain, and sleep architecture are especially vulnerable.
Liver Damage and Metabolic Harm
Your liver is the metabolic filter of your body. It breaks down toxins, metabolizes hormones and macronutrients, and supports immune function. Alcohol is metabolized in the liver into acetaldehyde, a highly reactive and toxic compound. Repeated exposure to acetaldehyde causes inflammation, fatty change, and eventually fibrosis and cirrhosis in susceptible individuals.
Chronic alcohol intake increases the risk of fatty liver disease, nonalcoholic fatty liver disease in some cases, alcoholic hepatitis, and cirrhosis. The good news is that the liver can start to heal within weeks of abstinence if structural damage has not advanced too far. Studies document significant improvement in liver enzymes and reductions in liver inflammation in heavy drinkers who abstain for just two to four weeks.

Alcohol Is a Carcinogen
This is nonnegotiable and important: alcohol is classified by international cancer authorities as a Group 1 carcinogen. That means there is sufficient evidence that alcohol causes cancer. The list of cancers includes mouth, throat, esophagus, liver, colon, and breast cancer. Even light to moderate drinking increases certain risks. For example, consuming one to six drinks per week increases a woman’s risk of breast cancer by about 24 percent according to several studies.
In 2024, large-scale analyses underscored alcohol as the third leading risk factor for cancer behind smoking and obesity. In the United States, alcohol contributes to tens of thousands of cancer cases per year. If your goal is longevity and reduced chronic disease risk, reducing alcohol intake is one of the highest-impact lifestyle changes you can make.
Sleep Architecture: REM, Slow Wave Sleep, and Recovery
Alcohol is commonly mistaken as a sleep aid because it often increases drowsiness and shortens the time it takes to fall asleep. That perceived benefit is deceptive. Alcohol disrupts sleep patterns. It reduces REM sleep, the critical stage for emotional regulation, memory consolidation, and learning. Alcohol also decreases slow wave sleep, the deepest restorative NREM stage necessary for physical recovery and immune function.
Regularly disrupting REM and slow wave sleep leads to chronic insomnia, worsened mood, and impaired cognitive function. Over time, poor sleep quality can raise inflammatory markers, reduce metabolic health, and impair glycemic control. For people who use alcohol to fall asleep, the long-term tradeoff is steep: worse sleep and worse recovery despite increased sleepiness.
Brain Atrophy, Dementia Risk, and Mood Disorders
Long-term alcohol consumption accelerates loss of brain tissue in regions tied to memory and learning. Excessive drinking increases the risk of dementia and contributes to depression and anxiety disorders. Even when drinking is not “heavy” by social standards, chronic exposure can subtly accelerate cognitive decline. The bottom line is that alcohol damages the physical substrate of cognition and emotional regulation, making it a major opponent of longevity and brain health.
Social Pressure, Habits, and the Hidden Costs
One of the main reasons alcohol consumption is so hard to reduce is social. Alcohol is woven into celebrations, networking, and date nights. The media normalizes it as a reward or a necessary component of adult social life. That social normalization obscures the health costs and makes cutting back psychologically difficult.
But the challenge is primarily social, not biological for most people. That means the highest-impact interventions are often behavioral and environmental. Change your default social activities. Set boundaries. Find substitutes. When I coach people, the first practical outcomes come from changing context more than from sheer willpower.
Benefits of Eliminating Alcohol: What You Can Expect
When you eliminate alcohol, improvements show up fast and continue to compound. The changes are measurable in days and dramatic within weeks.

Within days to weeks
- Improved hydration and fewer headaches
- Better sleep continuity and deeper REM and slow wave sleep
- Reduced daytime fatigue and clearer thinking
- Lowers acute inflammation and improves mood stability
For many people, the first week of abstinence brings noticeably better mental clarity and energy. People who track their sleep with HRV or sleep-tracking devices often see objective improvements in sleep stages and recovery metrics within a week.
Within two to four weeks
- Reduction in liver inflammation and improved liver enzyme profiles
- Improved skin quality and reduced facial puffiness
- More consistent energy patterns and stabilized blood sugar
- Reduced anxiety and improved sleep architecture
The liver is remarkably resilient. Studies document significant reductions in markers of liver inflammation for heavy drinkers who abstain for just a few weeks. That’s the clearest sign that recovery is possible and that the damage is not always permanent if addressed early.
Longer term
- Lowered risk of alcohol-related cancers over years of reduced exposure
- Reduced risk of liver cirrhosis and associated mortality
- Slower brain atrophy and reduced dementia risk
- Better metabolic health and reduced chronic disease burden
Everyone’s baseline risk is different. If you have a family history of liver disease or cancer, or preexisting metabolic disease, the benefit of alcohol reduction becomes even more pronounced. But even for healthy people, removing the steady source of inflammation and toxin exposure increases resilience, recovery, and biological age metrics.
How to Cut Alcohol Out: Practical, Stepwise Plan
Quitting alcohol can feel overwhelming. I recommend a pragmatic approach that combines behavior, environment, accountability, and physiological support. Here is a step-by-step plan you can implement today.
Step 1: Start Small and Build Momentum
One of my favorite lessons comes from a simple principle: choose the smallest unit you can reliably accomplish. If you are a daily drinker, commit to one alcohol-free day this week. Make that non-negotiable. Next week add another alcohol-free day. Small wins build confidence and neurochemical momentum. If you are already a light or weekend drinker, try a 30-day alcohol-free experiment to notice the difference.
Step 2: Set Clear Boundaries in Advance
Decide before you go into social situations what you will do. Precommitment dramatically reduces temptation. Options include:
- Drink sparkling water or a nonalcoholic beer for social rituals
- Designate yourself as the driver
- Use short scripts to deflect offers politely
When you decide ahead of time you reduce decision fatigue and social pressure becomes less influential.
Step 3: Replace Routines That Center on Alcohol
If your social life revolves around bars, intentionally curate alternatives. This could be outdoor activities, fitness classes, cooking nights, or board game evenings. New rituals become the default reward mechanisms for your brain, replacing the alcohol association.
Step 4: Track Progress and Celebrate Small Wins
Use a simple app or journal to track alcohol-free days, sleep quality, mood, and energy. Seeing progress over time is reinforcing and helps identify triggers or situations that cause relapse. Be kind to yourself. Recovery and behavior change are rarely linear.
Targeted Supplements and Nutrition Protocol: What I Recommend and Why
You asked for exact supplements and dosages. The guidance below is what I use clinically and personally to accelerate recovery after reducing or eliminating alcohol. These recommendations are designed to support liver function, replenish depleted nutrients, restore sleep, protect cognition, and stabilize mood. They are not a replacement for medical care. If you have liver disease, take medications, or are pregnant or breastfeeding consult a physician before starting any supplement.
Immediate Support: Days 1–7
The first week is about supporting detox pathways, preventing abrupt deficiencies, restoring hydration, and improving sleep. Use these baseline supplements concurrently and follow the dosing guidelines.
- Hydration and Electrolytes: Use a balanced electrolyte formula each day. I recommend adding a rehydration tab to a liter of water each morning and after any exercise. Example product: electrolyte tabs with sodium, potassium, magnesium, and chloride. No exact grams here because formulations vary but look for a balanced sodium 200–400 mg, potassium 100–200 mg per serving profile.
- Thiamine (Vitamin B1): 300 mg per day for the first 7–14 days, then reduce to 100 mg per day. Thiamine is the most commonly depleted B vitamin in heavy drinkers and is essential for energy metabolism and brain health. For people with a history of heavy use or symptoms like confusion, clinicians often use higher doses or IM injections. I recommend oral thiamine 300 mg split into morning and evening doses initially.
- B-Complex: A high-potency B-complex once daily. Look for a formula that includes B2, B3, B5, B6, folate (as methylfolate), and B12 as methylcobalamin. These support hepatic metabolism and nervous system recovery. Typical doses: B6 25–50 mg, methylfolate 400–800 mcg, B12 500–1000 mcg sublingual daily.
- Magnesium Glycinate: 200–400 mg at night. Magnesium supports sleep, relaxation, and nervous system stability. Glycinate is well tolerated and less likely to cause loose stools.
- Vitamin C: 1000 mg daily. Supports antioxidant activity and immune function during early recovery.
- N-Acetylcysteine (NAC): 600 mg twice daily for the first two weeks, then 600 mg daily for maintenance if desired. NAC supports glutathione synthesis and helps the liver deal with oxidative stress.
- Milk Thistle (Silymarin): Standardized silymarin 150 mg three times daily or 300 mg twice daily. Milk thistle is hepatoprotective and supports liver regeneration.
- Omega-3 EPA/DHA: 1–2 grams combined EPA/DHA daily. Omega-3s support brain recovery, reduce systemic inflammation, and improve mood.
- Probiotic: A multi-strain probiotic with Lactobacillus and Bifidobacterium strains, 10–50 billion CFU daily. Alcohol alters gut microbiota; restoring it supports systemic health and mood.
These are foundational items I suggest starting immediately. They address the biggest and most common nutritional deficits and provide antioxidant and metabolic support while the body clears alcohol-derived toxins.
Weeks 2–8: Recovery and Repair Phase
After the initial week, shift the focus to rebuilding reserves, optimizing sleep, and protecting cognition.
- Vitamin D3: 2000–5000 IU daily depending on baseline. Check serum 25(OH)D and aim for mid-normal range. Vitamin D supports immune function, mood, and metabolic health.
- Zinc: 15–30 mg daily. Zinc supports immune function and is often depleted with alcohol use. Do not exceed 40 mg daily long-term without medical supervision.
- S-Adenosylmethionine (SAMe): 400 mg twice daily for 4–8 weeks if you have persistent mood or liver support needs. SAMe supports methylation and liver function. Use caution if you have bipolar disorder and consult your doctor.
- Liposomal Glutathione: 250–500 mg daily. Glutathione replenishment supports hepatic detoxification and antioxidant defenses.
- Lion’s Mane Mushroom: 500–1000 mg twice daily. Lion’s mane supports neurogenesis and cognitive recovery in some studies.
- Bacopa Monnieri: 300 mg daily standardized extract. Bacopa supports memory and cognitive processing as the brain recovers.
- Creatine Monohydrate: 3–5 g daily. Creatine supports brain energy metabolism and helps cognitive performance during recovery.
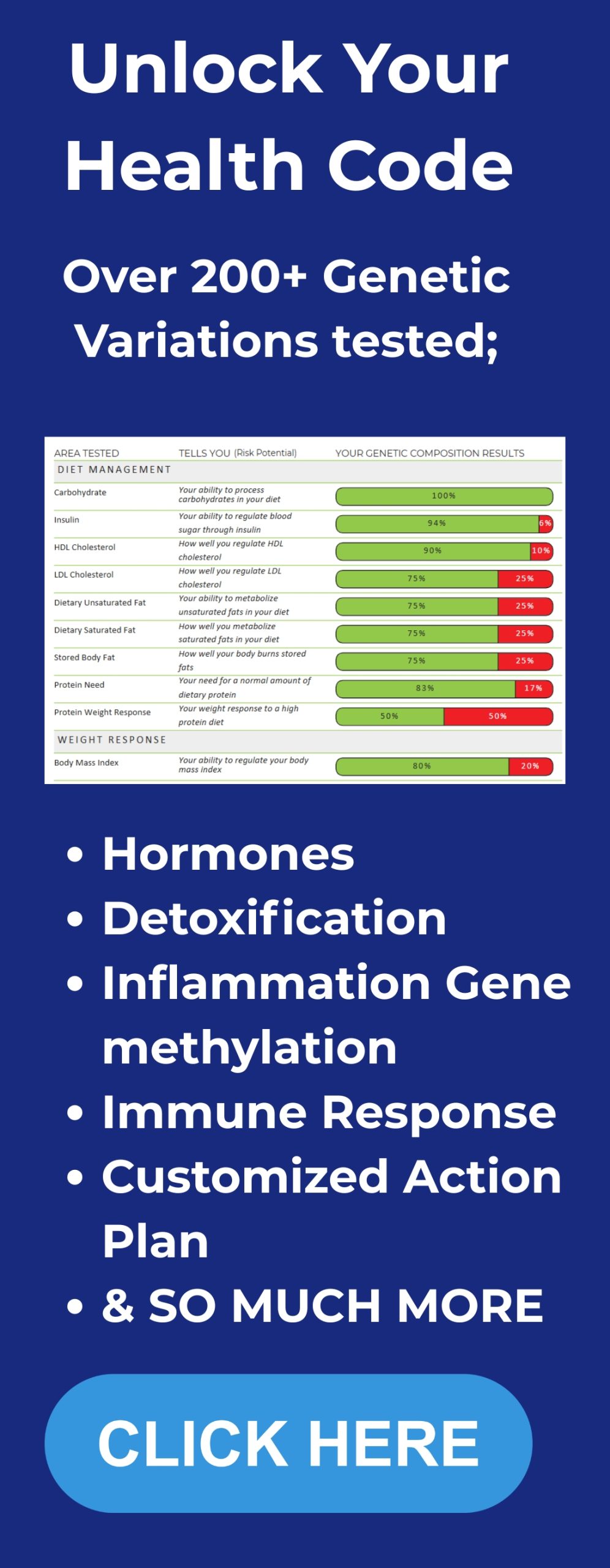
Nutrition is essential. Prioritize protein-rich meals, leafy greens, cruciferous vegetables, and foods high in B vitamins such as legumes, eggs, and lean meats. Avoid processed sugars that worsen liver load and mood swings. Get personalized DNA insights.
Ongoing Maintenance: Months 2–12
Once you have stabilized, you want a maintenance stack that supports long-term resilience and reduces cancer, cognitive, and metabolic risk factors.
- Multivitamin: A high-quality multivitamin that includes bioavailable folate, B12, and minerals to cover daily needs.
- Omega-3s: Continue 1–2 g EPA/DHA daily.
- Vitamin D3: Maintain individualized dose per lab values.
- Probiotic: Continue but consider cycling strains and occasional prebiotic fiber.
- Periodic NAC: 600 mg daily on a maintenance basis if desired.
- Routine Liver Labs: Check liver enzymes, CBC, and metabolic panel every 3–6 months during recovery and annually thereafter.
Supportive lifestyle changes are equally critical: regular resistance training to preserve muscle mass and metabolic health, consistent sleep routines, stress management, and reduced processed foods. I emphasize the combination of behavioral change with targeted supplementation because each element multiplies the others.
How to Implement This Protocol Safely
Supplements are tools. They are not a magical fix.Explore the full range of BetterLife Protocols products to support your recovery.
Here is how I recommend implementing them safely.
- Start with hydration and B vitamin foundation immediately. Thiamine, B-complex, magnesium, and NAC are my priority for the first week.
- Get baseline labs: liver enzymes (ALT, AST), GGT, bilirubin, fasting glucose, HbA1c, lipids, vitamin D, and complete blood count. If possible, check B12 and folate. Repeat these labs at 4–12 weeks to track progress.
- Avoid excessive supplement overlap. If you take a high-dose multivitamin check the B vitamin content before stacking a separate B-complex.
- Monitor for side effects. If you experience GI upset, reduce doses or change forms (e.g., magnesium citrate versus glycinate).
- If you are on prescription medications or have serious liver disease consult a physician before starting NAC or SAMe.
In my experience, following these steps while removing alcohol from your routine produces the fastest and safest improvements. The goal is restoration, not extreme short-term cleansing that stresses the body.
Behavioral Tools That Amplify Success

Supplements help physiology. Behavior changes ensure long-term adherence. Here are my practical behavioral tools that transform early gains into lasting lifestyle changes.
1. Use Small, Non-Negotiable Habits
Small, repeatable actions beat grand plans. My favorite is the one-day-at-a-time approach. Declare one alcohol-free day per week for a month. Then increase frequency. Keep the behavior simple so it becomes automatic.
2. Change Your Social Script
Have a few go-to responses so you don’t have to justify your choices in social settings. Nonalcoholic beer or mocktails make it easy to blend in. Being the designated driver is a socially acceptable way to avoid drinking that also builds social capital.
3. Replace Reward Triggers
Alcohol often functions as a reward. Replace it with new rewarding rituals that support health: a 20-minute walk after work, a warm bath, a call with a friend, a healthy snack you enjoy, or a brief breathwork session. Rewiring reward systems is critical for long-term change.
4. Track and Reflect
Use a simple journal to record mood, sleep, cravings, and energy. Over time you will see patterns: certain evenings, stressors, or social contexts that trigger use. Tracking turns vague motivation into concrete behavior change.
5. Build a Supportive Environment
Tell close friends or family about your plan and ask for their support. If that’s not possible, consider online communities or a coach. Accountability increases the odds of lasting change.
Check out our BetterLife Integrate program for structured support and accountability tools.
Common Questions I Get and Practical Answers
Is one glass of wine per night really that bad?
Every choice involves tradeoffs. A single glass of wine has acute effects on sleep and cognitive consolidation and contributes to cumulative alcohol exposure. For some people, the social and psychological benefits may feel worth it. From a pure longevity perspective, any regular alcohol intake increases risk for specific cancers and contributes to wear on liver and brain repair systems. If longevity and optimized health are your primary goals, removing even small regular amounts of alcohol is beneficial.
Will supplements prevent liver disease if I continue to drink?
No. Supplements can support liver function and reduce some oxidative stress, but they are not protective against the severe consequences of ongoing heavy drinking. The only reliably protective action against alcohol-related liver disease is reducing or stopping alcohol intake. Supplements are supportive adjuncts for recovery and for people who are reducing, not for people who intend to continue heavy consumption.
How quickly will I notice improvements in sleep and energy?
Many people notice improved sleep quality, deeper REM cycles, and clearer energy within the first week of abstinence. Objective sleep-tracking metrics usually show improvements in sleep stages within a few nights to a week. Energy and mood improvements often continue to increase over the first month as liver inflammation drops and sleep improves.
Are nonalcoholic beers and wines safe?
Nonalcoholic beers and wines are better than their alcoholic counterparts when it comes to ethanol exposure. However, some contain trace alcohol and can be high in sugar and calories. Use them as transitional tools if they help you maintain abstinence, but be mindful of ingredient quality.
What if I have tried to quit and relapsed?
Relapse is common in behavior change and does not mean failure. Use it as data. Identify the triggers and rebuild your plan. Consider an accountability partner, reduce exposure to high-risk environments, and lean into the physiological support protocol above during high-risk periods. If you have moderate to severe dependence, seek medical supervision and consider professional addiction services.
My 8-Week Action Plan
If you want a practical roadmap to put this into motion, follow this eight-week plan I use with clients and personally recommend to friends.
- Week 1: Choose one alcohol-free day, start hydration and electrolytes, begin thiamine 300 mg/day, B-complex once daily, magnesium at night, NAC 600 mg twice daily, and begin a probiotic.
- Week 2: Increase to two alcohol-free days, add milk thistle 150 mg three times daily, continue vitamins and electrolytes, begin daily movement routine (20–30 minutes).
- Week 3: Aim for three alcohol-free days, add omega-3 1–2 g daily, start lion’s mane 500 mg twice daily if cognitive support is desired, and track sleep nightly.
- Week 4: Try a 30-day alcohol-free challenge if you can. Reassess labs: liver enzymes and vitamin D. Continue supplement stack and increase sleep hygiene measures.
- Week 5: Re-evaluate social triggers, shift at least one drinking social activity to a non-drinking alternative, and keep daily supplements.
- Week 6: If you completed a 30-day break, extend to 60 days. Add SAMe 400 mg twice daily only if you have ongoing mood or liver concerns and after consulting a clinician.
- Week 7: Continue maintenance supplements, reduce B1 to 100 mg/day after physician approval if you were on high dose, and keep tracking sleep and mood.
- Week 8: Review labs, celebrate progress, and plan long-term maintenance (vitamin D, omega-3, probiotic, occasional NAC). Consider a lifestyle upgrade like consistent resistance training and a Mediterranean-style diet to maximize longevity benefits.
FAQ
Do these supplements interact with medications?
Some supplements interact with prescription drugs. For example, SAMe can influence serotonin pathways and may interact with antidepressants. NAC can interact with nitroglycerin in rare cases. SAMe and some herbal products may have contraindications in bipolar disorder. Always consult a medical provider before starting supplements if you take medications or have serious health conditions.
Is complete abstinence necessary for everyone?
Not necessarily. Risk is dose-dependent and individual. Some people choose to reduce rather than eliminate alcohol and still achieve large health gains. If your goal is maximal longevity and minimal cancer risk, the safest approach is elimination. If your priority is harm reduction and quality of life, a carefully managed reduction plan combined with monitoring might be best for you.
How do I know if I have an alcohol use disorder?
If you experience cravings, loss of control, withdrawal symptoms, or continued use despite negative consequences, you may meet criteria for alcohol use disorder. This is a medical condition and is best addressed with professional support, which can include counseling, medication-assisted treatment, and medical detox if needed.
Where can I find the supplements and protocols you recommend?
I share detailed protocols and product guides at Betterlifeprotocols.com. There you can find the supplement formulations I prefer, provider resources, and step-by-step checklists to support your journey.
Final Thoughts: Small Changes, Big Results
Cutting alcohol out of your life is not about depriving yourself of pleasure. It is about investing in the one asset that determines your ability to experience and contribute over the long run: your health. The science is clear. Alcohol disrupts sleep, impairs cognitive function, increases cancer risk, damages the liver, and accelerates brain atrophy. But the most important fact I want to leave you with is this: change is possible and the benefits compound quickly.
Start with one small action today. Pick an alcohol-free day, begin a basic supplement stack with thiamine, B-complex, magnesium, and NAC, and choose one social habit to replace with a healthier alternative. Track your sleep and energy for a week and notice how your body responds.